Cell Death Differ:TRIM22通过加速IκBα降解激活NF-κB信号
2020-09-01 QQY MedSci原创
NF-κB信号转导通路最初被发现表征于免疫系统中,现已发现其与癌症发生发展中的许多特征相关,这些特征包括细胞增殖、血管生成和对治疗的抵抗力。与其他恶性肿瘤一致的是,在人胶质母细胞瘤(GBM
NF-κB信号转导通路最初被发现表征于免疫系统中,现已发现其与癌症发生发展中的许多特征相关,这些特征包括细胞增殖、血管生成和对治疗的抵抗力。与其他恶性肿瘤一致的是,在人胶质母细胞瘤(GBM)中同样观察到NF-κB的高组成性活性,并可以促进该疾病的间充质分化和治疗耐药性。然而目前其相关的分子机制还有待研究。
三序基(TRIM)蛋白家族,是RING型E3泛素连接酶的一个亚家族,能够通过调节NF-κB的转录活性充当包括GBM在内的多种癌症发生发展过程中的关键调节因子。在该研究中,研究人员旨在探究TRIM蛋白在GBM发生发展过程中的作用,通过使用NF-κB驱动的荧光素酶报告基因系统和公共数据库的筛选,研究人员确定了TRIM22是GBM细胞中NF-κB信号的潜在激活因子。
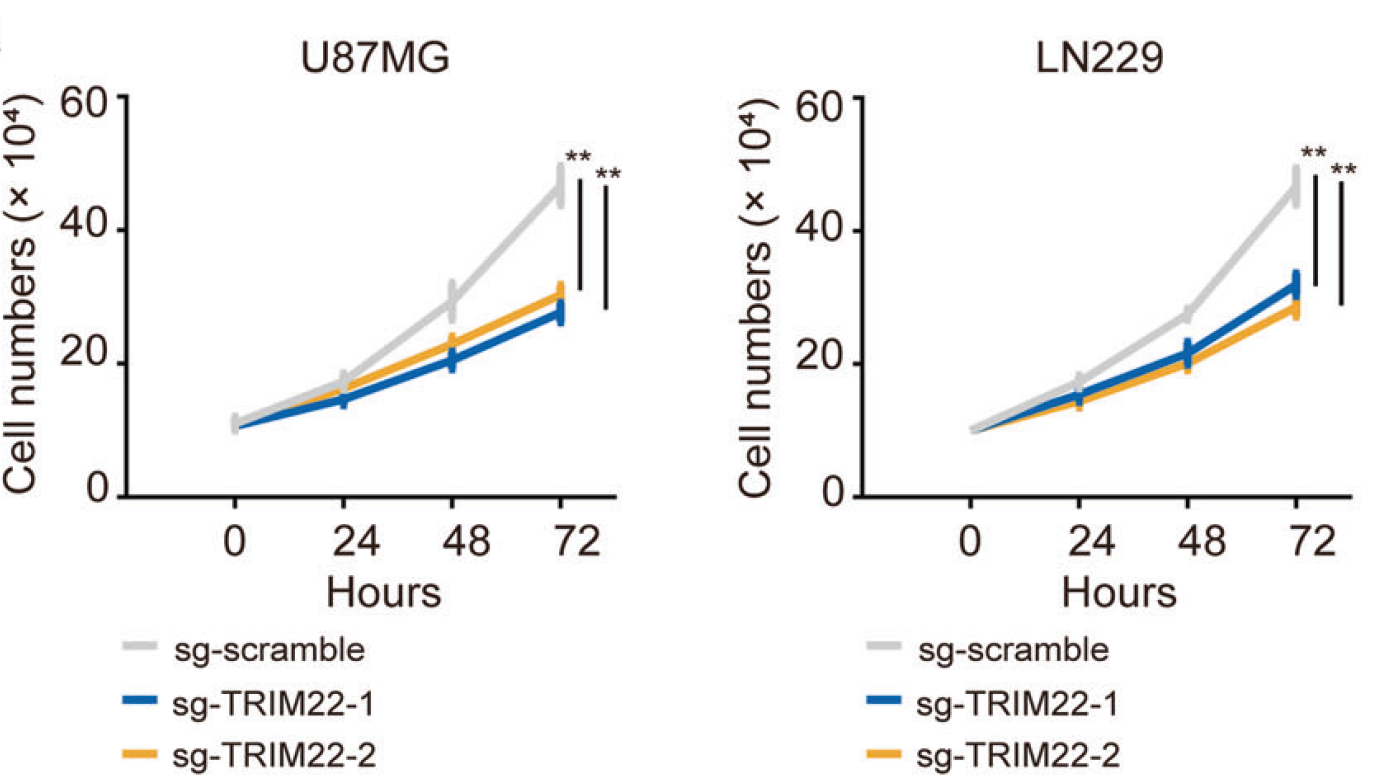
体外实验和原位移植瘤模型研究显示,通过Cas9-sgRNA技术敲除TRIM22会导致GBM细胞增殖减少,而过表达TRIM22则能够增强细胞增殖能力。
研究人员发现TRIM22蛋白的两个突变体:一个是蛋白关键RING-finger结构域缺失,另一个则是RING E3连接酶(C15/18A)的两个活性位点的氨基酸改变,均不能促进GBM细胞增殖过程,说明TRIM22的E3连接酶活性具有促进细胞增殖的特性。
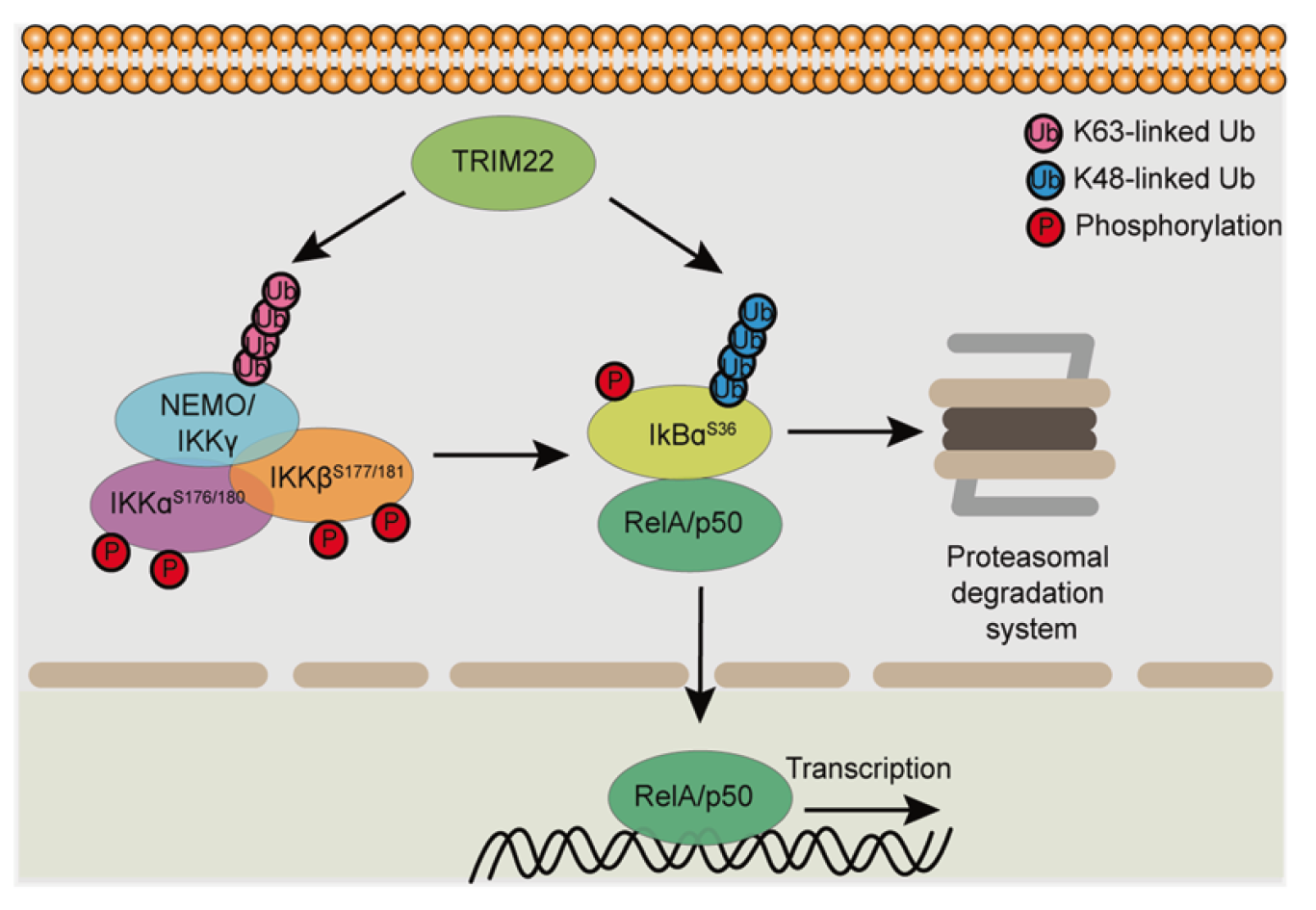
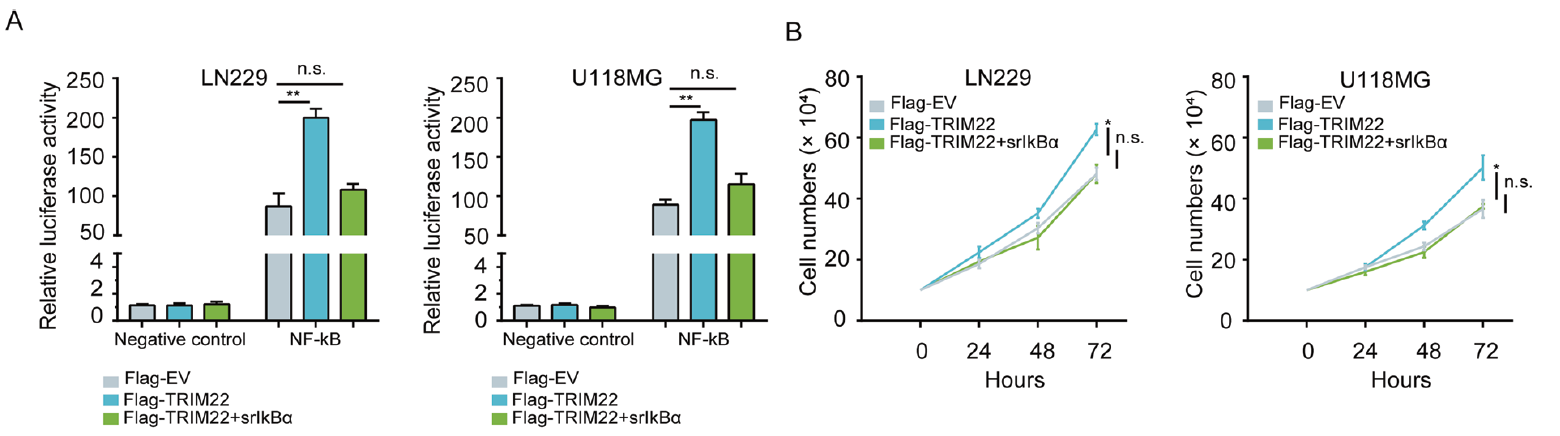
免疫共沉淀实验显示,TRIM22能够通过结合NF-κB负调节因子IκBα诱导K48连接的泛素化途径从而加速其降解。TRIM22还能够与NF-κB上游调节因子IKKγ形成复合物,促进K63连接的泛素化途径并诱导IKKα/β和IκBα的磷酸化。当在GBM细胞系中表达非磷酸化的突变体srIκBα则会抑制TRIM22的促增殖作用。
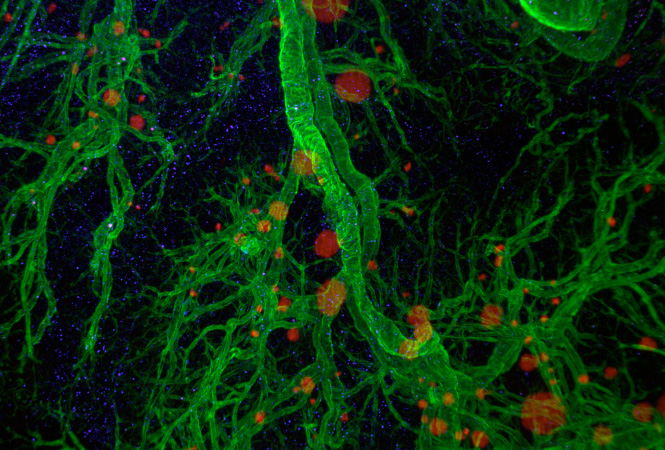
最后,GBM样本的组织芯片分析结果显示TRIM22的表达水平升高,且TRIM22的高表达水平与进行性神经胶质瘤的临床参数相关。
总而言之,该研究结果显示,在人胶质母细胞瘤中,TRIM22能够通过翻译后修饰NF-κB信号通路中的两个关键调节因子来激活NF-κB信号。
原始出处:
Ji, J., Ding, K., Luo, T. et al. TRIM22 activates NF-κB signaling in glioblastoma by accelerating the degradation of IκBα. Cell Death Differ (19 August 2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Differ#
19
#CEL#
30
👍
82
#Cell#
32
学习
84
#Death#
35
学习
90