根据冠状动脉病变的部位、范围、血管阻塞程度和心肌供血不足的发展速度、范围和程度的不同,分为五种临床类型:一、无症状型冠心病;二、心绞痛型冠心病;三、心肌梗死型冠心病;四、缺血型心肌病型冠心病;五、猝死型冠心病。

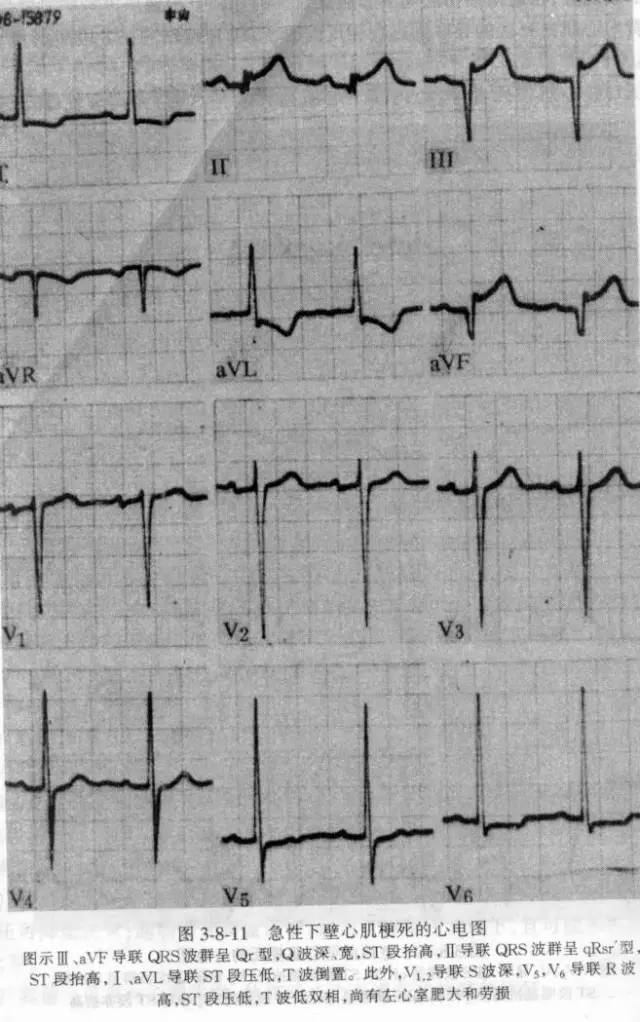
一 急性心肌梗死的心电图诊断
(一)特征性改变
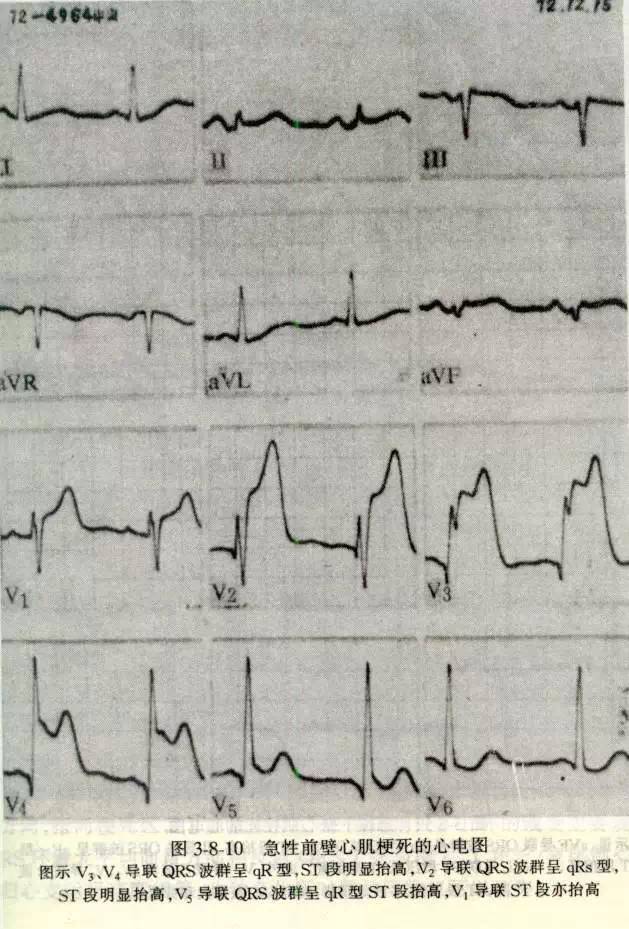
典型急性心肌梗死心电图诊断的三要素:
1、病理性Q波(坏死改变)
(1)Q波增宽>0.04S
(2)Q波加深>1/4 R Q波出现粗钝与切迹
2、ST段弓背向上抬高 (损伤改变)
3、T波倒置(缺血改变)
(二)、心电图的动态演变及分期
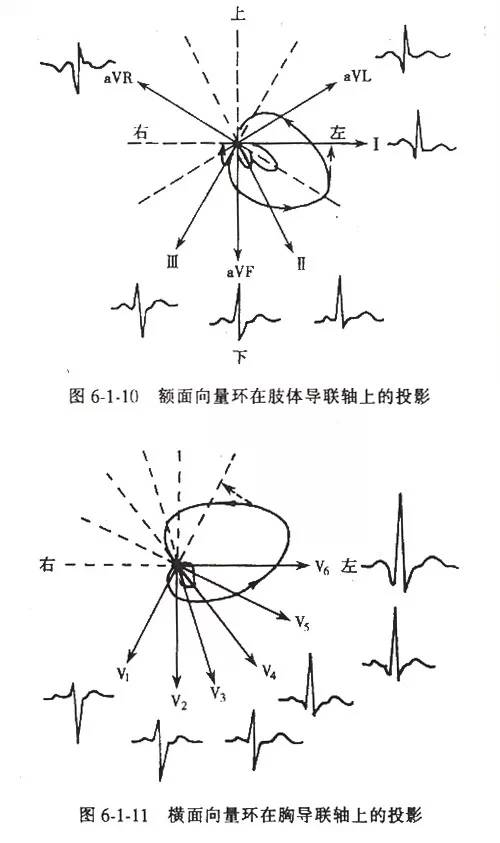
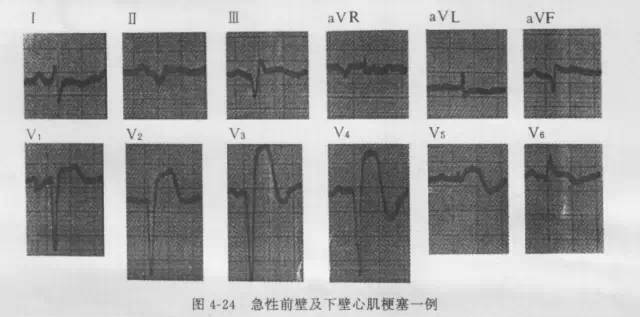
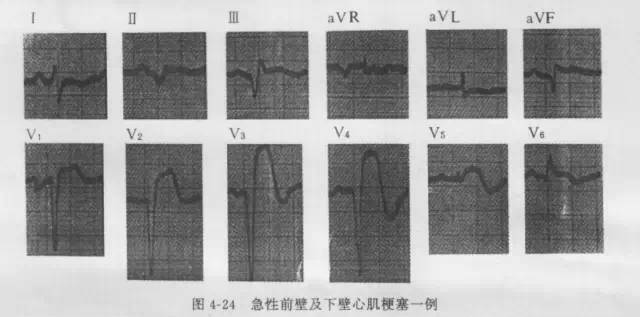
(三)、心肌梗死的定位诊断
-
前间壁:V1、V2、V3
-
前壁:V3、V4、V5
-
广泛前壁:V2~V5(V1)(V6)
-
高侧壁:Ⅰ、AVL
-
侧壁:V5、V6、V7
-
下壁:Ⅱ、Ⅲ、AVF
-
正后壁:V7、V8、V9
-
右室:V3R、V4R、V5R
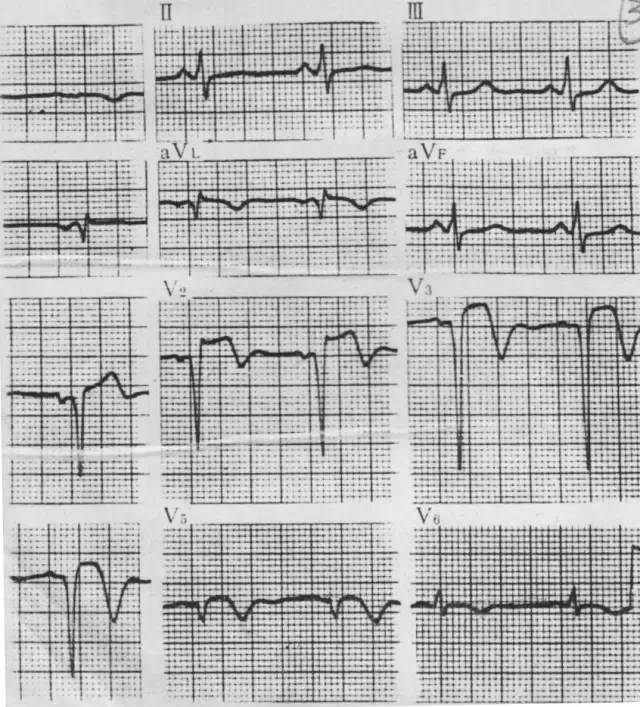
二 不典型心肌梗死
(一)、非Q波型心肌梗死:
(非透壁性心肌梗死)
1、普遍导联ST段较显著的抬高或压低。
2、T波双向或倒置,双肢对称,有时仅见T波改变,出现巨大而倒置的T波ST波,并有动态变化。
3、不出现病理性Q波
4、临床症状及酶学检查符合心肌梗死改变
(二)、右室心肌梗死
1、V3R、V4R、V5R 导联ST段抬高,T波倒置并出现病理性Q波。
2、均合并下壁、后壁心肌梗死。
3、临床可有右心功能不全的体征和血流动力学障碍。
(三)、心房梗死
当心室肌梗死合并有下列心电图改变,可考虑同时有心房梗死的可能。
1、P-R段移位:升高或压低。
2、P波增宽、粗钝、畸形并有动态变化。
3、在血流动力学稳定的情况下,出现较为持久的房性心律失常。
4、常伴有其他心肌梗死的表现
(四)、持续性ST段抬高的心肌梗死
三 慢性冠状动脉供血不足
(一)、心电图复极变化
(二)、心电图除极变化
1、QRS波群增宽,电压降低。
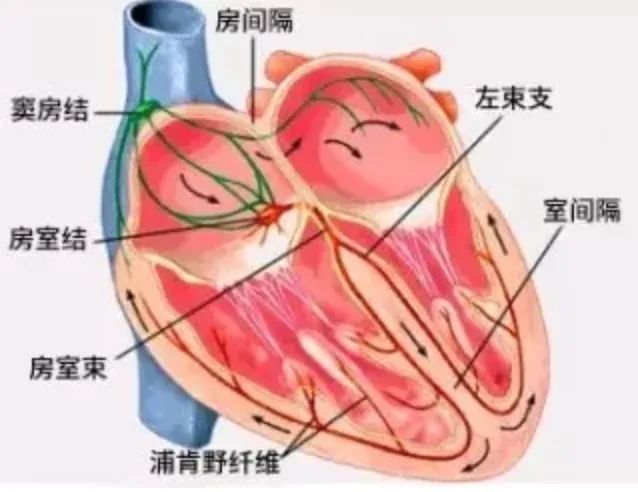
2、传导阻滞:房室传导阻滞、完全性或不完全性左右束枝阻滞、房内阻滞等。
3、心律失常:各种早搏及心房颤动,以室早最为常见。
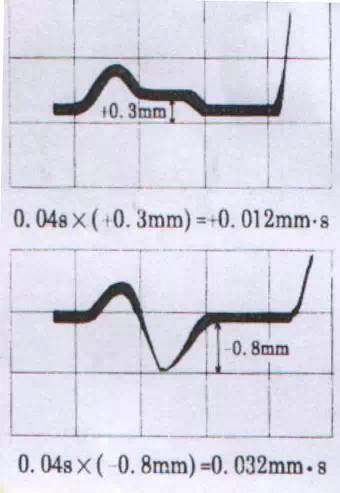
4、PTF-V1负值增大。
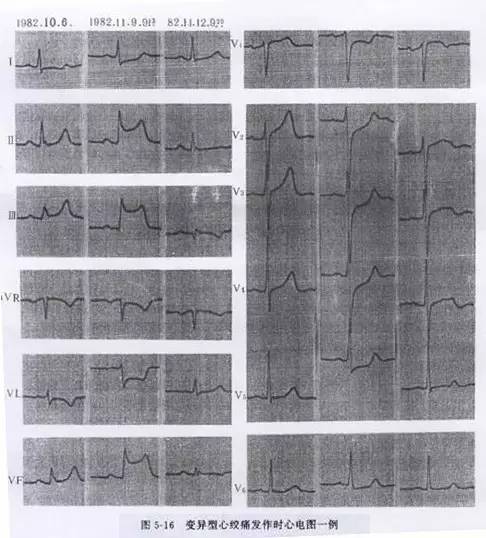
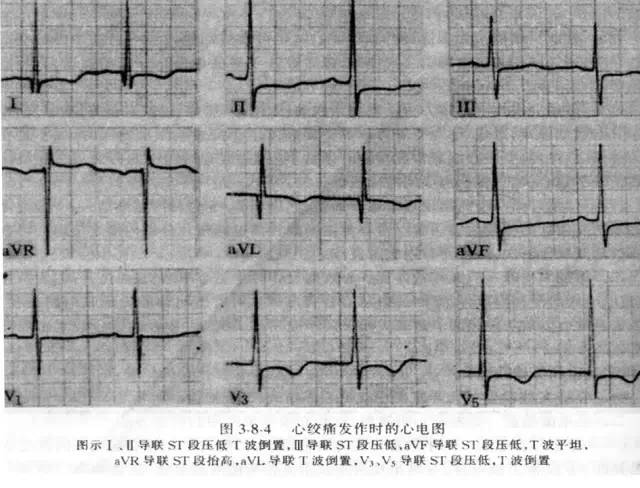
四 心绞痛(急性冠状动脉供血不足)
五 诊断慢性冠状动脉供血不足
心电图的辅助试验
(一)、活动平板运动试验
1、适应症
(1)对不典型胸痛或可疑冠心病病人进行鉴别诊断;(2)评估冠心病病人的心脏负荷能力;(3)评价冠心病的药物或手术治疗效果;(4)进行冠心病易患人群流行病调查筛选实验。
2、禁忌症
(1)急性心肌梗死;(2)不稳定心绞痛;(3)心力衰竭;(4)中、重度瓣膜病或先天性心脏病。(5)严重的肺部疾患或高血压,血压超过160/100mmHg以上者;(6)急性心包炎、心肌炎、严重主动脉瓣狭窄;(7)年老体衰、行动不便、骨骼、关节等疾患。
3、阳性标准
(1)运动中或运动后出现ST段缺血型下移≥0.1mV,持续时间>2分钟;(2)运动中出现心绞痛;(3)出现严重心律失常;(4)ST段抬高,很少见。
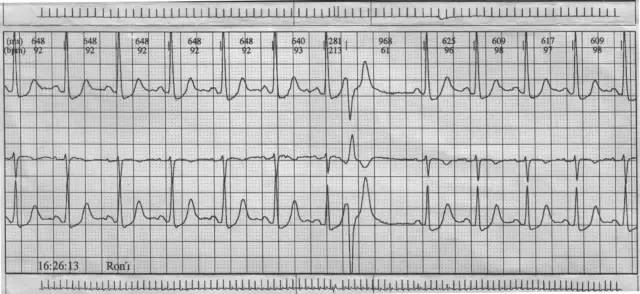
(二)、动态心电图
1、临床应用范围
(1)心悸、气促、头昏、晕厥、胸痛等症状性质的判断;(2)心肌缺血的诊断和评价,尤其是发现无症状心肌缺血的重要手段;(3)心律失常的定性和定量诊断;(4)药物的疗效评价;(5)选择安装起搏器的适应症、评价起搏器的功能。
2、心肌缺血的DCG诊断
ST段水平型或下垂型下移>0.1mV,持续时间1min,2次间隔1min以上。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













学习了
60
学习了
54
学习了
41
#鉴别诊断#
0
学习了,谢谢总结
61
不错,学习了
55
学习
53