Burns Trauma:非严重烧伤会增加小鼠的癌症发病率,并对T细胞的激活和功能产生长期影响
2022-05-20 医路坦克 MedSci原创
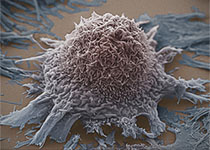
烧伤患者因感染、精神健康状况、心血管疾病和癌症出院后多年因烧伤本身而住院的风险增加,在非严重烧伤后4周,与使用B16黑色素瘤原位模型的对照组相比,小鼠更容易发生肿瘤。
最近的证据表明,烧伤患者因感染、精神健康状况、心血管疾病和癌症出院后多年因烧伤本身而住院的风险增加。烧伤也被证明会导致持续的免疫系统功能障碍。免疫功能的这种变化可能导致观察到的慢性病风险的增加。然而,烧伤创伤后扰乱长期免疫功能的机制及其与长期发病率的联系仍不清楚。在这项研究中,我们使用非严重烧伤的小鼠模型研究了烧伤后免疫功能的变化。
已建立的小鼠非严重烧伤模型(相当于8%总体表面积的全层烧伤)与B16黑色素瘤原位模型相结合,研究了烧伤与癌症之间的联系。考虑到CD8+T细胞在这个模型中是有效的肿瘤抑制的重要驱动因素,我们也使用烧伤合并单纯疱疹病毒感染的小鼠模型研究了这种免疫群体潜在的失调。用流式细胞术检测和量化感兴趣的细胞群和免疫功能的变化。
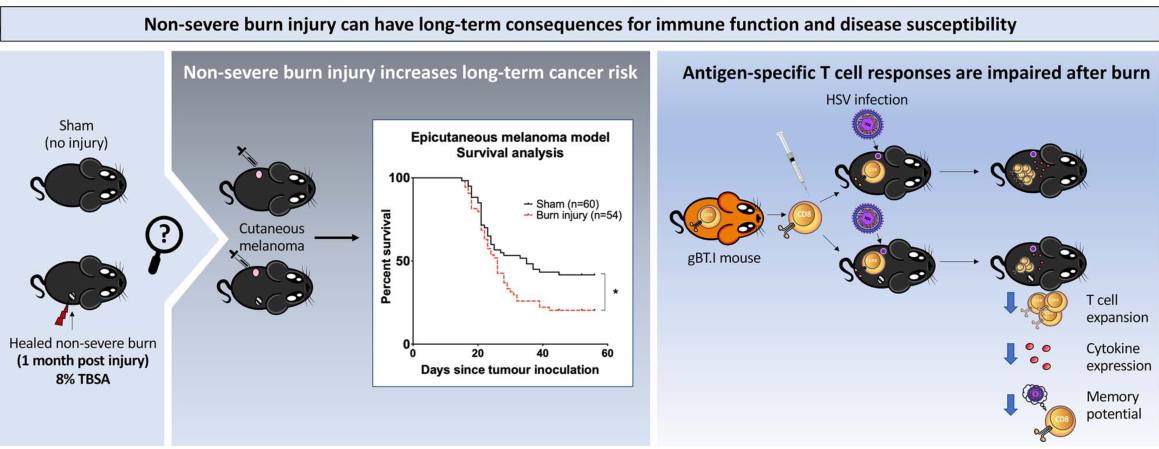
我们证明,在非严重烧伤后4周,与使用B16黑色素瘤原位模型的对照组相比,小鼠更容易发生肿瘤。此外,我们的结果显示,烧伤后1个月CD8+T细胞的增殖、分化和记忆能力明显受损。
我们的数据提示,即使在非严重烧伤后,CD8+T细胞介导的免疫功能也可能在持续一段时间内功能失调。在患者中进行进一步的研究以验证这些发现,可能会支持临床干预,以恢复或保护烧伤后患者的免疫力,并降低观察到的继发性疾病增加的风险。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#发病率#
0
#TRA#
37
#长期影响#
37
学习
45
#Trauma#
48