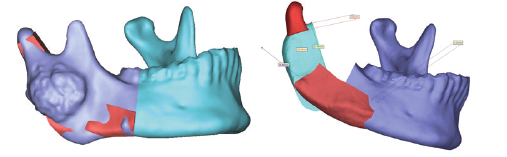
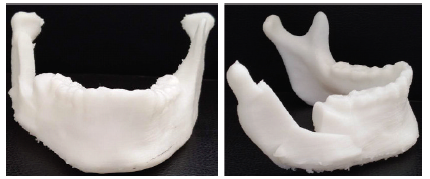
应用3D打印技术修复重建下颌骨骨化纤维瘤切除术后缺损1例
2019-06-10 徐超 卢利 中国实用口腔科杂志
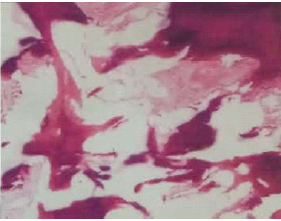
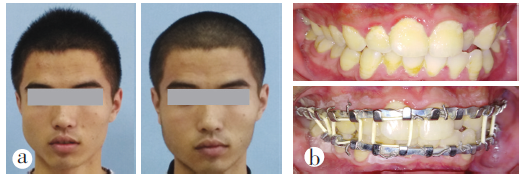
患者男,18岁,9年前行右侧下颌支肿物切除术,术后病理回报“青少年骨化纤维瘤”,近年来自觉面部再次膨隆,并逐渐加重,于2017-08-08来中国医科大学附属口腔医院口腔颌面外科门诊就诊,拍摄上下颌骨3D -CT发现下颌支肿物,门诊以“右下颌骨肿物”为诊断收入院。


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#骨化纤维瘤#
38
#下颌#
26
#3D打印技术#
28
#切除术#
31
#3D#
29
#纤维瘤#
22
#下颌骨#
29