Nat Commun:新辅助抗OX40疗法(MEDI6469)治疗头颈部鳞状细胞癌患者的临床研究
2021-02-26 xiaozeng MedSci原创
头颈部鳞状细胞癌(HNSCC)作为全球第七大常见的癌症,其特征是具有较高的治疗耐药性。
头颈部鳞状细胞癌(HNSCC)作为全球第七大常见的癌症,其特征是具有较高的治疗耐药性。尽管包括外科手术、放疗和化疗在内的积极治疗对该疾病显示出了一定的疗效,然而局部晚期HNSCC患者的复发率仍高达为50%。
既往研究显示,靶向PD-1(程序性死亡受体1)或PD-L1(程序性死亡配体1)的检查点抑制剂(CI)抗体可有效的改善转移性HNSCC患者的总体生存率,且已被FDA批准与化疗药物联用治疗。然而,只有10%到20%的患者受益于PD-1/PD-L1阻断治疗。
靶向其他途径,如共刺激分子(OX40、GITR和4-1BB等),可以增强荷瘤宿主中T细胞的免疫力。先前尚未有相关研究探索免疫共刺激激动剂在癌症患者新辅助治疗中的作用。
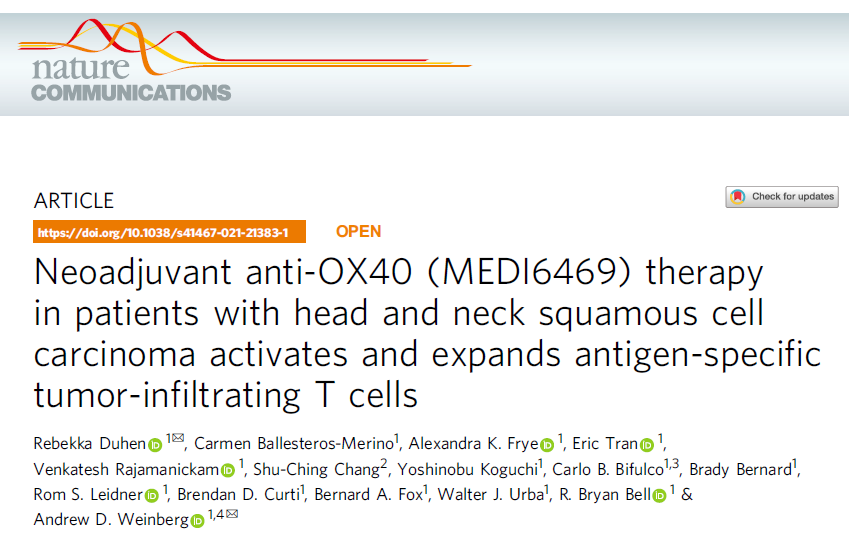
抗OX40治疗后肿瘤和间质淋巴细胞浸润的变化
在该研究中,研究人员报道了一项Ib期临床试验(NCT02274155)的结果,该试验中共17例局部晚期HNSCC患者在手术切除之前接受了鼠抗人OX40激动剂抗体(MEDI6469)。临床试验的主要终点为确定抗OX40新辅助疗法的安全性和可行性。次要终点为评估抗OX40对肿瘤和血液中淋巴细胞亚群的影响。
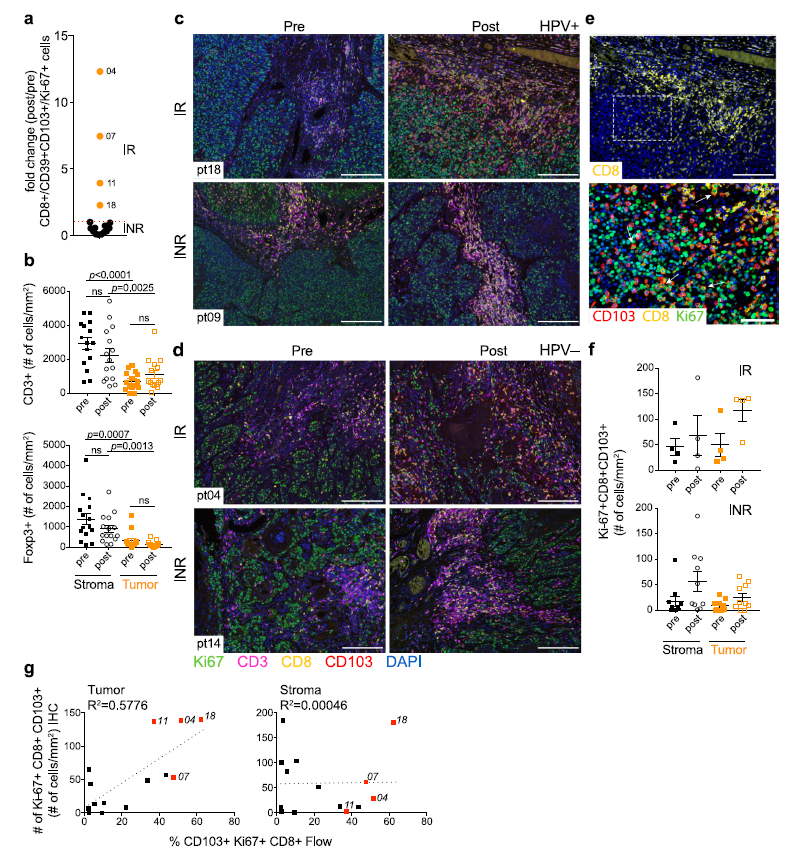
结果显示,新辅助抗OX40疗法的耐受性良好,没有延迟手术的进行,并最终达到了试验的主要终点。外周血表型数据显示,抗OX40给药两周后CD4+和CD8+T细胞增殖增加。治疗前后肿瘤活检比较显示,大多数患者的活化的常规CD4+肿瘤浸润淋巴细胞(TIL)有所增加。对CD8+TIL的分析显示,在25%的具有可评估肿瘤组织(N=4/16)的患者中,肿瘤抗原反应性提高、处于增殖的CD103+ CD39+细胞数量增加,且这些患者均保持无病状态。
新辅助抗OX40治疗后患者的生存率分析
总而言之,该研究结果显示,抗OX40疗法在术前是安全的,可以增加血液和肿瘤中CD4+和CD8 + T细胞的活性和增殖能力。该研究也表明,肿瘤反应性CD103+ CD39+ CD8+ TIL的增加可能是抗OX40临床活性的潜在生物学标记。
原始出处:
Duhen, R., Ballesteros-Merino, C., Frye, A.K. et al. Neoadjuvant anti-OX40 (MEDI6469) therapy in patients with head and neck squamous cell carcinoma activates and expands antigen-specific tumor-infiltrating T cells. Nat Commun 12, 1047 (16 February 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#OX40#
35
#COMMUN#
31
#细胞癌#
25
#Nat#
38
#新辅助#
27
临床试验的主要终点为确定抗OX40新辅助疗法的安全性和可行性。次要终点为评估抗OX40对肿瘤和血液中淋巴细胞亚群的影响。
68
靶向其他途径,如共刺激分子(OX40、GITR和4-1BB等),可以增强荷瘤宿主中T细胞的免疫力。先前尚未有相关研究探索免疫共刺激激动剂在癌症患者新辅助治疗中的作用。
81
既往研究显示,靶向PD-1(程序性死亡受体1)或PD-L1(程序性死亡配体1)的检查点抑制剂(CI)抗体可有效的改善转移性HNSCC患者的总体生存率,且已被FDA批准与化疗药物联用治疗。然而,只有10%到20%的患者受益于PD-1/PD-L1阻断治疗。
78
#头颈部鳞状细胞癌#
40
#头颈部#
37