Cancers:手术和射频消融(RFA)治疗乙肝相关肝细胞癌患者的疗效对比
2021-12-05 yd2015 MedSci原创
研究表明,早期肝细胞患者射频消融(RFA)治疗的OS与手术切除治疗相当,但是RFS短于手术切除治疗。
手术切除和射频消融治疗早期肝癌的有效性仍然存在争议。此外,以往的研究没有考虑抗病毒治疗相关因素,尽管现在有确凿的证据表明抗病毒治疗对确定慢性乙型肝炎相关肝癌患者的预后至关重要。因此,来自韩国团队开展了回顾性研究,比较乙肝相关肝细胞癌患者手术和射频消融(RFA)治疗的预后。相关结果发表在Cancers杂志上。
研究纳入761例患者为医院队列,567例(74.5%)患者行手术切除(切除术组),194例(25.5%)患者行射频消融(RFA组)。RFA组肿瘤平均大小较小(1.7 cm vs. 3.9 cm, p<0.01)以及BCLC 0期患者的比例较高(58.8% vs. 16.0%,p<0.01)。同时,肝硬化患者的比例更高(85.6% vs 63.1%,p<0.01)。经过IPTW匹配后,RFA组的肿瘤仍较小(2.3 vs. 3.4 cm, p<0.01);中位甲胎蛋白(AFP)水平更低 (9.9 vs. 17.6 ng/mL, p = 0.01)。
纳入1277例患者为全国人群队列,手术切除925例(72.4%),射频消融352例(27.6%)。与医院队列相似,射频消融组的肿瘤平均大小较小(1.8 cm vs. 3.7 cm, p <0.01),即使在使用IPTW后也不平衡(1.8 vs. 3.8 cm, p <0.01;SMD = 0.99)
在整个医院队列中,在81.0(62.3 107.1)个月的随访期间,两组的中位OS均未达到,切除组中位RFS为71.7个月,RFA组40.7个月。应用IPTW前,RFA组与切除组的OS无差异(HR = 0.738, 95% CI = 0.435 1.250, P = 0.26)。而RFA组与更短的RFS相关(HR = 1.268,95% CI = 1.024–1.571, p = 0.03)。
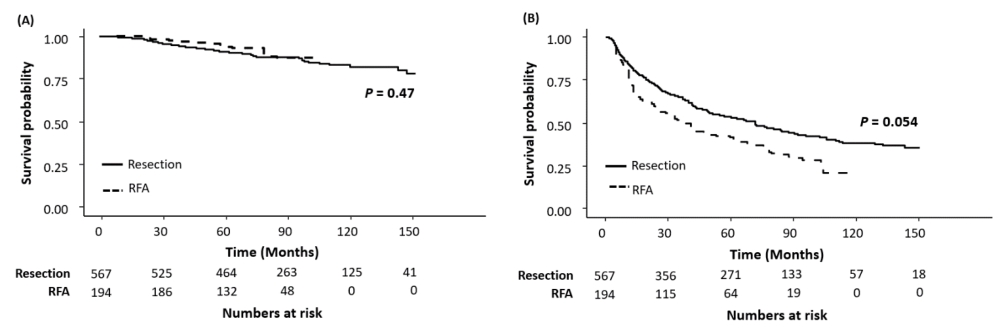
医院队列的OS和RFS
采用IPTW平衡基线特征后,两者的OS无显著统计学差异(HR = 0.774, 95% CI 0.368-1.630, p = 0.50);同样RFA组与更短的RFS相关(HR = 1.491, 95% CI 1.034-2.149, p = 0.03)。调整相关因素后,两组OS同样没有统计学差异(aHR = 0.870, 95% CI = 0.400–1.897, p = 0.73),RFA组与更短的RFS相关(aHR = 1.562, 95% CI = 1.099–2.219, p = 0.01)。但是在IRTW加权患者中,两组的OS(log-rank p = 0.47)和RFS (log-rank p = 0.054)都没有统计学差异。抗病毒治疗是OS (aHR = 0.444, 95% CI = 0.251–0.786, p = 0.01)和RFS (aHR = 0.544, 95% CI = 0.391–0.757, p < 0.01)独立良好预后因素。

多因素分析预后相关因素
<3cm患者亚组分析中,253例(60.2%)患者行手术切除,167例(39.8%)患者行射频消融治疗。RFA组的平均肿瘤较小(1.6 cm vs. 2.1 cm),但其肝硬化患者比例较高(85.6% vs. 72.7%) (p<0.01)。IPTW平衡后,两组的OS同样也没有统计学差异(HR = 0.735,95% CI = 0.336–1.610 , p = 0.44)。RFA组与更短的RFS相关(40.7 vs. 90.6个月, log-rank p = 0.03;HR = 1.628, 95% CI = 1.114–2.379, p = 0.01)。抗病毒治疗是OS (aHR = 0.289, 95% CI = 0.141–0.585, p < 0.01) 和RFS (aHR = 0.538,95% CI = 0.372–0.776, p < 0.01) 独立良好预后因素。
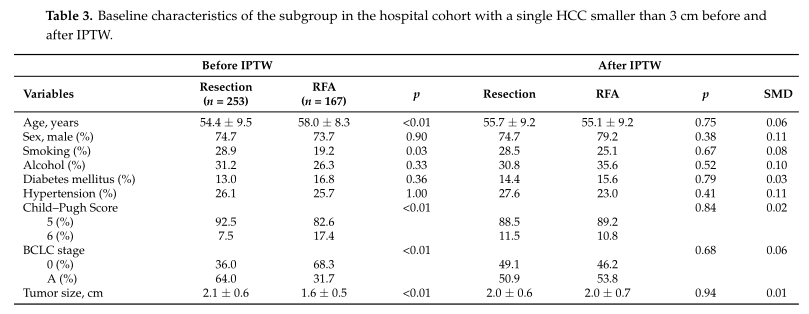
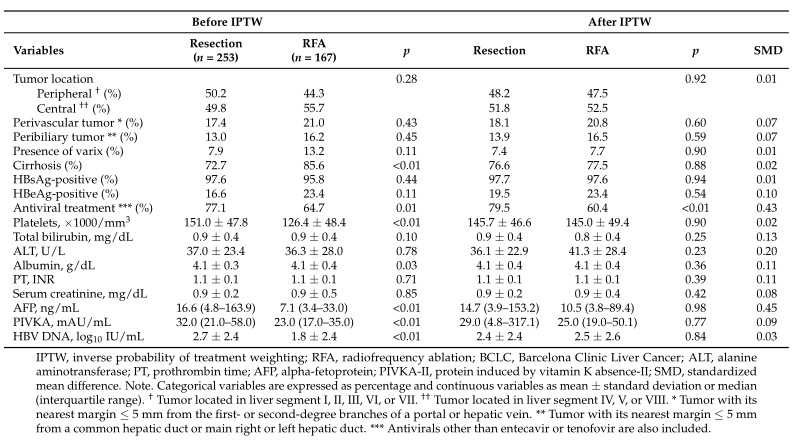
<3cm肝细胞癌临床特征
在全国队列中,两组的OS同样也没有统计学差异(aHR = 0.981, 95% CI = 0.661–1.456, p = 0.92)。

全国队列OS
切除组(26.3%)并发症的总发生率高于RFA组(13.9%),包括发热、肿瘤、出血、脓肿和门静脉血栓(p<0.01)。RFA组的中位住院时间(3天)明显短于切除组(12天)(p <0.01)。
综上,研究表明,早期肝细胞患者射频消融(RFA)治疗的OS与手术切除治疗相当,但是RFS短于手术切除治疗。
原始出处:
Hur, M.H.; Lee, J.-H.; Kim, J.Y.; Hong, J.H.; Park, M.K.; Cho, H.J.; Choi, N.R.; Kim, J.; Kim, M.A.; Nam, J.Y.; et al. Comparison of Overall Survival between Surgical Resection and Radiofrequency Ablation for Hepatitis B-Related Hepatocellular Carcinoma. Cancers 2021, 13, 6009. https://doi.org/10.3390/ cancers13236009
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#ERS#
35
#细胞癌#
38
#肝细胞#
38
#射频消融#
50
#消融#
47