European Radiology:VSASL技术在脑胶质瘤定性、定量分析的应用
2022-06-03 shaosai MedSci原创
血管生成是侵袭性肿瘤增殖、浸润和转移的必要条件,因此较高的肿瘤血管是诊断、分级和治疗反应评估的重要生物标志物。
 胶质瘤约占原发性脑肿瘤的80%,5年生存率差异很大,从少突胶质瘤的81%、弥漫性星形细胞瘤的50%到胶质母细胞瘤的6%不等。尽管临床在了解其发病机制和分子遗传学方面取得了重大进展,但胶质瘤仍然是治疗难度最大的恶性肿瘤之一。
胶质瘤约占原发性脑肿瘤的80%,5年生存率差异很大,从少突胶质瘤的81%、弥漫性星形细胞瘤的50%到胶质母细胞瘤的6%不等。尽管临床在了解其发病机制和分子遗传学方面取得了重大进展,但胶质瘤仍然是治疗难度最大的恶性肿瘤之一。
血管生成是侵袭性肿瘤增殖、浸润和转移的必要条件,因此较高的肿瘤血管是诊断、分级和治疗反应评估的重要生物标志物。因此,关于肿瘤灌注特征的先进成像技术对于胶质瘤的术前特征分析具有附加价值,有助于手术规划,提供预后信息,对于手术后的靶向治疗和监测治疗反应也特别重要。
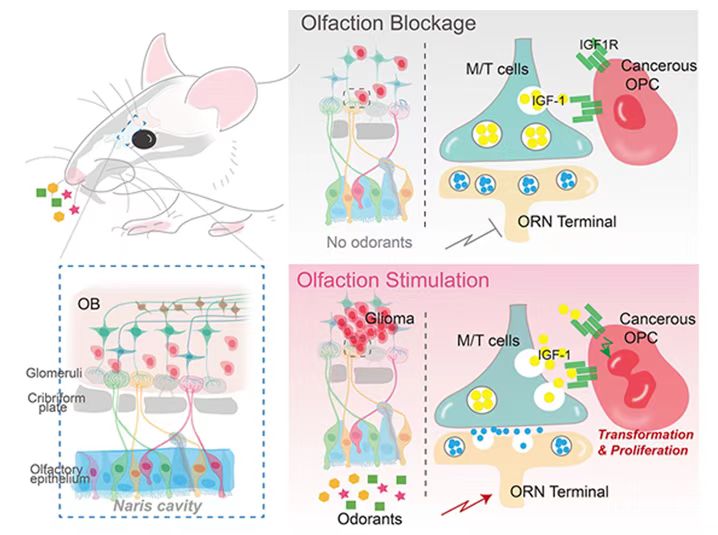
DSC-PWI技术通过使用钆基对比剂产生相对脑血容量(CBV)和脑血流量(CBF)的体内图谱,并在许多临床研究中显示了肿瘤灌注的精确特征。动脉自旋标记(ASL)可在无需对比剂的情况下测量灌注信号,因此具有很大的临床前景。现阶段,临床引入了速度选择性(VS)ASL技术,可通过标记血管树中所有流速高于小动脉血管截断速度的上游血液,并将时间延迟敏感性降到最低。
近日,发表在European Radiology杂志的一项研究通过术前对PCASL和DSC-PWI进行比较,并进一步比较了其与术后组织病理学分级的关系,评估了这种新兴的VSASL技术在胶质瘤患者中的诊断表现,并进行了定性和定量评估。
本研究对2017年至2019年期间接受术前灌注MRI包括VSASL、PCASL和DSC-PWI的44名新诊断胶质瘤患者进行了回顾性评价。根据1-5分的标准,目测评估肿瘤相对于灰质的信号强度,并使用加权卡帕评估VSASL或PCASL与DSC-PWI之间的配对一致性。相对肿瘤血流(rTBF)是通过对血流图上的肿瘤内热点区域取样测量的,并与对侧正常灰质血流进行归一化。进行线性回归和Bland-Altman分析以评估ASL方法和DSC-PWI之间rTBF测量的相关性和一致性。构建ROC分析以确定三种灌注方法对胶质瘤分级的诊断性能。
与PCASL相比,VSASL得出的TBF图在视觉上与DSC-PWI更具可比性(加权卡帕为0.90 vs 0.68)。在定量分析中,VSASL-rTBF与DSC-PWI值的相关性高于PCASL-rTBF(R2 = 80% vs 47%,两者的P < 0.001)。ASL和DSC衍生的rTBF都显示出对低级和高级胶质瘤的良好区分(p < 0.001)。与PCASL相比,VSASL在胶质瘤分级中产生了更高的诊断敏感性、特异性和准确性。

图 a 34岁女性,右额叶胶质母细胞瘤(WHO IV级,IDH野生型,O6-MGMT甲基化),显示FLAIR高信号,反映了肿瘤的高细胞性、不规则、异质性增强、中心坏死。PCASL、VSASL和DSC-PWI的CBF图具有可比性,都显示出一个明显的灌注增加的边缘(白色箭头),对应于肿瘤的实性增强部分。 b 一位50岁的女性,左额顶胶叶质母细胞瘤(WHO IV,IDH野生型,MGMT未定型)显示FLAIR高心哈后和扩散性降低,但有轻度增强和中心坏死。在CBF图上,VSASL与DSC-PWI相比,在肿瘤-组织对比上更具有可比性,显示肿瘤区域(箭头)和顶叶皮质的灌注增加,内侧无增强的细胞病灶灌注轻度升高(箭头)
本研究表明,VSASL是一种强大的灌注技术,与DSC-PWI相比,在视觉评估和灌注定量方面与PCASL的一致性更高。在胶质瘤分级中,VSASL与PCASL相比也显示出更高的诊断敏感性、阴性预测值和准确性,可提高ASL对胶质瘤患者TBF的准确、无创定量的诊断性能。
原文出处:
Yaoming Qu,Dexia Kong,Haitao Wen,et al.Perfusion measurement in brain gliomas using velocity-selective arterial spin labeling: comparison with pseudo-continuous arterial spin labeling and dynamic susceptibility contrast MRI.DOI:10.1007/s00330-021-08406-7
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#定量分析#
24
#VSA#
33
#PE#
28
#SAS#
28
#ASL#
31