SERCA2氧化还原C674的取代通过激活IRE1α/XBP1s通路促进肺血管重塑
2022-06-28 网络 网络
肺动脉高压(PH)是一种以肺血管重构为特征的危及生命的疾病,其中肺动脉平滑肌细胞(PASMCs)的过度增殖起着重要作用。研究阐明了 C674 氧化失活对肺血管重塑和 PH 发展的因果影响。
肺动脉高压(PH) 是一种危及生命的疾病,静息时平均肺动脉压 (PAP) ≥ 25 mmHg。PH临床上分为五组。第 1 组是肺动脉高压 (PAH),其他都与各种疾病有关。PAH 是一种特别严重和渐进的形式,临床起病缓慢,渐进恶化,其特征是丛状病变。肺血管重构是PH的主要原因。由于 PH 患者的肺样本有限且缺乏合适的动物模型来模拟人类 PH,因此 PH 的发病机制仍存在争议。
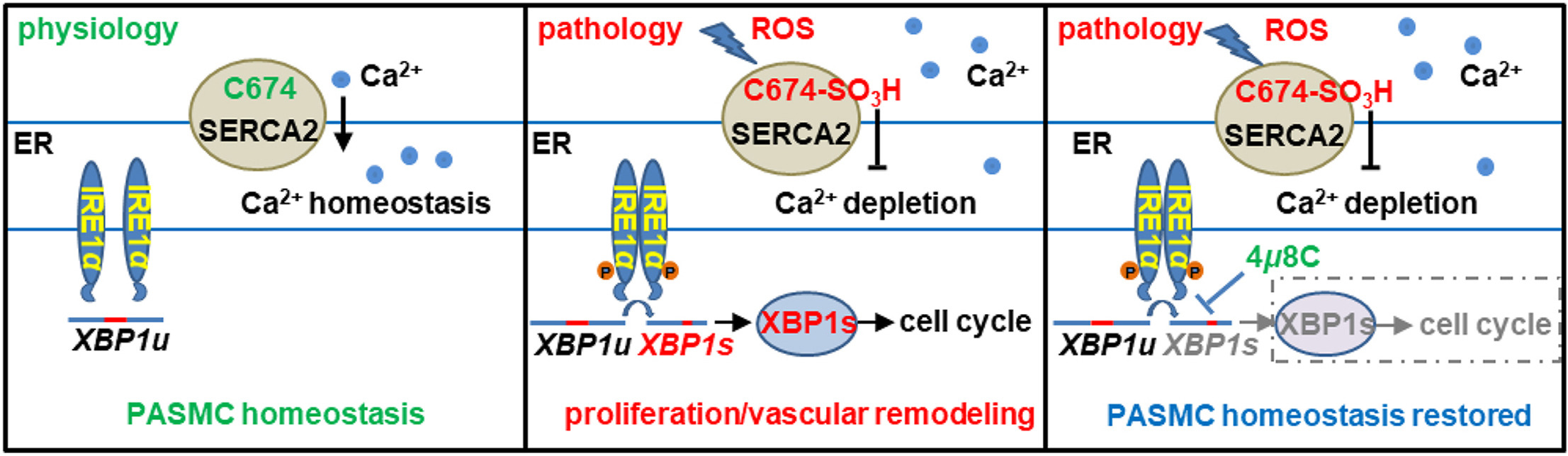
肌质/内质网 Ca 2+ ATP 酶 (SERCA)通过将 Ca2+从细胞质转运到肌质网 (SR) 和内质网 (ER)来维持 Ca2+稳态,以维持细胞质中的低 Ca2+ 浓度和SR/ER 中的高 Ca2+浓度。SERCA2(小鼠基因Atp2a2 ,人基因ATP2A2)是血管SERCA的主要亚型,主要包括Atp2a2a和Atp2a2b基因型,其中Atp2a2b是管家基因。半胱氨酸674(C674)的S-谷胱甘肽化在生理条件下调节SERCA2的活性,但在活性氧(ROS)增加的病理情况下,这种修改被其不可逆的氧化所阻止。细胞内 Ca2+水平升高是众所周知的平滑肌细胞 (SMC) 增殖的原因。SERCA2活性的抑制诱导缺氧肺静脉重塑。SERCA2a 的减少与野百合碱诱导的大鼠肺动脉 (PA) 重塑有关。C674 及其氧化失活和 SERCA2b 在肺血管重塑中的作用仍不清楚。在这里,我们使用杂合SERCA2C674S 敲入小鼠 (SKI),其中 C674 被丝氨酸(S674) 取代,表明部分 C674 氧化失活。结果表明,SKI 发生了类似于人类 PH 的显著肺血管重塑,并且其右心室收缩压 (RVSP) 随着年龄的增长而适度增加。在肺动脉平滑肌细胞 (PASMCs) 中,S674 取代 C674 通过激活需要酶 1 α (IRE1α )和剪接 X-box 结合蛋白 1 (XBP1s) 途径的肌醇来加速细胞周期并促进细胞增殖。类似于 SERCA2a 9, SERCA2b 对于抑制 PASMCs 的增殖也很重要。本研究提供了一种 SERCA2 功能障碍促进 PASMC 增殖的新机制,即通过激活 IRE1α / XBP1s 通路,并首次证实抑制 IRE1α / XBP1s 通路可防止肺血管重塑。
图文说明:
半胱氨酸674(C674)是维持内质网(ER)Ca2+平衡的关键。它的不可逆氧化通过激活肌醇需求酶1α(IRE1α)/拼接的X-box结合蛋白1(XBP1s)通路而引起肺血管重塑。抑制IRE1α/XBP1s通路可抑制C674失活引起的肺血管重塑。
研究结果:
1.缺氧会增加SERCA2 C674的不可逆氧化,并减少肺和PASMCs中SERCA2的含量;
2.用S674取代C674会增加右心室压力并诱发肺血管重塑;
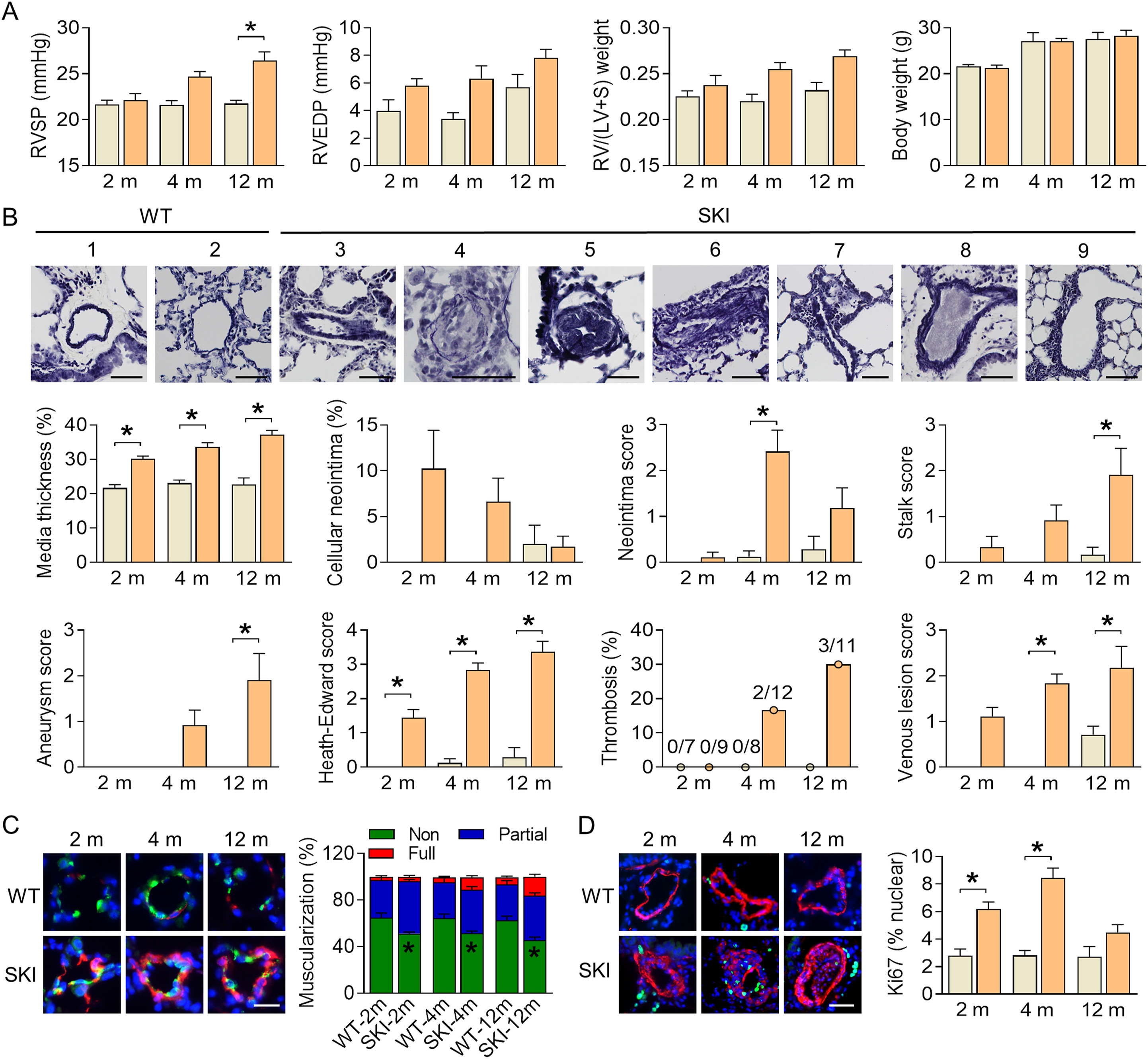
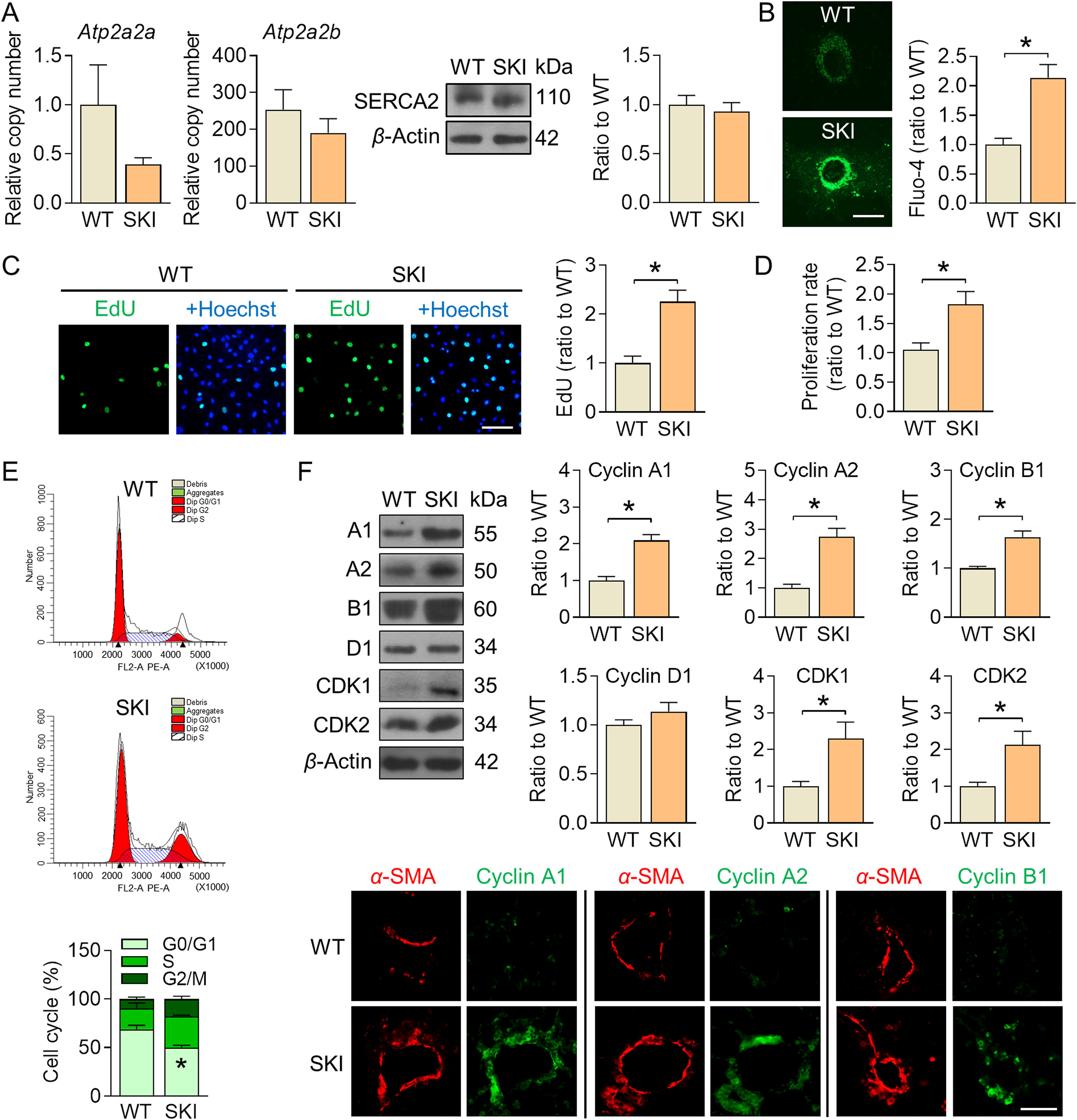
3.用S674取代C674,通过加速细胞周期促进PASMC增殖;
4.用S674取代C674诱导ER压力以促进PASMC增殖;
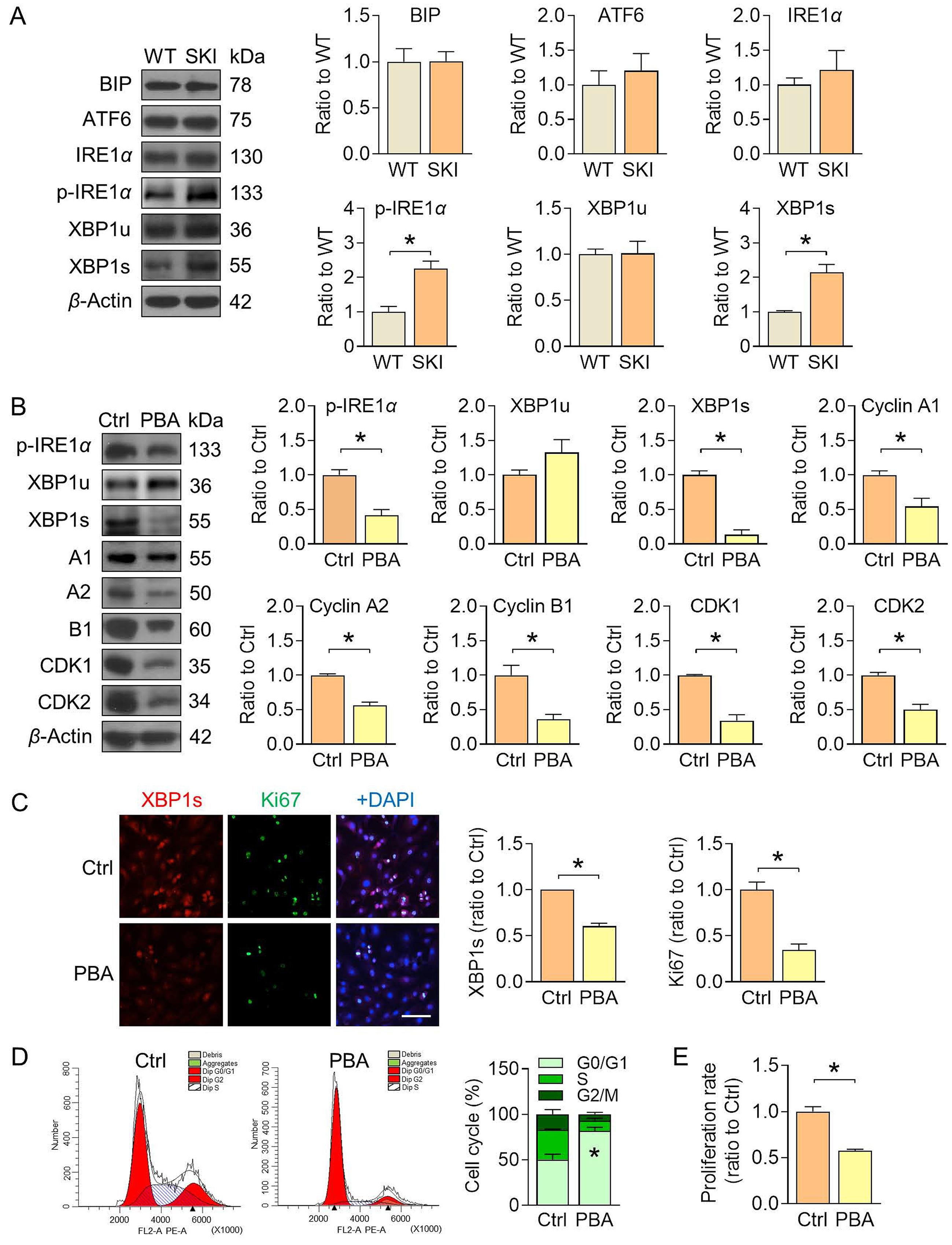
5.XBP1s的上调促进SKI PASMC的增殖;

6.抑制IRE1α/XBP1s途径可抑制SKI PASMC增殖;

7.抑制IRE1α/XBP1s途径可防止SKI肺血管重塑;

8.SERCA2b抑制IRE1α/XBP1s通路和SKI PASMCs的增殖;

研究结论:
SERCA2中的C674,特别是SERCA2b,通过抑制IRE1α/XBP1s途径的激活来限制PASMC的增殖,从而维持肺血管的稳态。SKI发生的肺血管重塑在组织学上与PH患者相似,可能成为肺血管重塑和PH的病因研究和药物筛选的重要工具。SERCA2 C674的氧化失活及其下游的IRE1α/XBP1s途径的激活可能是各种PH的共同机制之一。IRE1α/XBP1s途径和SERCA2可能是PH治疗的潜在目标。
参考文献:
Yu W, Xu G, Chen H, Xiao L, Liu G, Hu P, Li S, Kasim V, Zeng C, Tong X. The substitution of SERCA2 redox cysteine 674 promotes pulmonary vascular remodeling by activating IRE1α/XBP1s pathway. Acta Pharm Sin B. 2022 May;12(5):2315-2329. doi: 10.1016/j.apsb.2021.12.025. Epub 2022 Jan 5. PMID: 35646520; PMCID: PMC9136575.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#血管重塑#
49
#XBP1#
49
#氧化还原#
53
#XBP1s#
40
精彩评论,需要您登录查看
74
#CA2#
33