European Urology:胰岛素血症和炎症性饮食模式与前列腺癌的风险
2021-01-12 MedSci原创 MedSci原创
高胰岛素血症和炎症是相互关联的途径,它们将饮食与几种慢性疾病的风险联系起来。有证据表明,这些途径也可能增加前列腺癌的风险。
发达国家的前列腺癌负担明显高于低收入国家,从低收入水平国家移民到高收入水平国家的男性发病率也会升高,这表明饮食和生活方式因素可能在该疾病的病因学中起作用。然而,已知的危险因素仅限于老年、血统、家族史和某些遗传因素。仍然迫切需要确定可改变的风险因素,以帮助指导预防战略。
迄今为止,大多数关于饮食和前列腺癌发病率的研究都集中在个体饮食成分上。虽然有证据表明某些食物和营养物质与前列腺癌有关,如乳制品增加前列腺癌风险和番茄红素降低前列腺癌风险,但许多其他单独的饮食因素显示没有结果。膳食模式评估是一种替代方法,它提供了更好地考虑添加剂效应和膳食成分之间复杂的相互作用的优势。饮食模式也允许多种方法来实现健康饮食,并越来越多地被用于制定饮食建议。另一个使饮食和前列腺癌研究复杂化的因素是该疾病的生物学异质性,有证据表明惰性癌和侵袭性癌在病因学上存在差异。
高胰岛素血症和炎症是两个相互关联的生物学途径,将饮食与几种癌症的风险联系起来,研究表明,这些也可能增加前列腺癌的风险。
近日,European Urology上新发表的一项研究为了确定高胰岛素血症饮食和炎症饮食是否与前列腺癌发病率和死亡率相关,研究者在美国男性的前瞻性队列研究中调查了基于这些途径的两种以经验假设为导向的饮食模式与前列腺癌的总体风险,以及根据临床分期、Gleason评分和致死结果更有侵袭性的疾病形式之间的关系。
研究者在卫生专业人员随访研究(1986 - 2014)中,前瞻性地随访了4209名男性。通过基线时的食物频率问卷计算两种有效饮食模式的得分,每4年更新一次。评估总体、晚期和致死性前列腺癌的预后。采用Cox比例风险回归法,确定了两种经验假设导向的饮食模式之间的多变量校正风险比(HRs)和95%置信区间(CIs),即高胰岛素血症的经验饮食指数和经验饮食炎症模式与前列腺癌风险之间的关系。
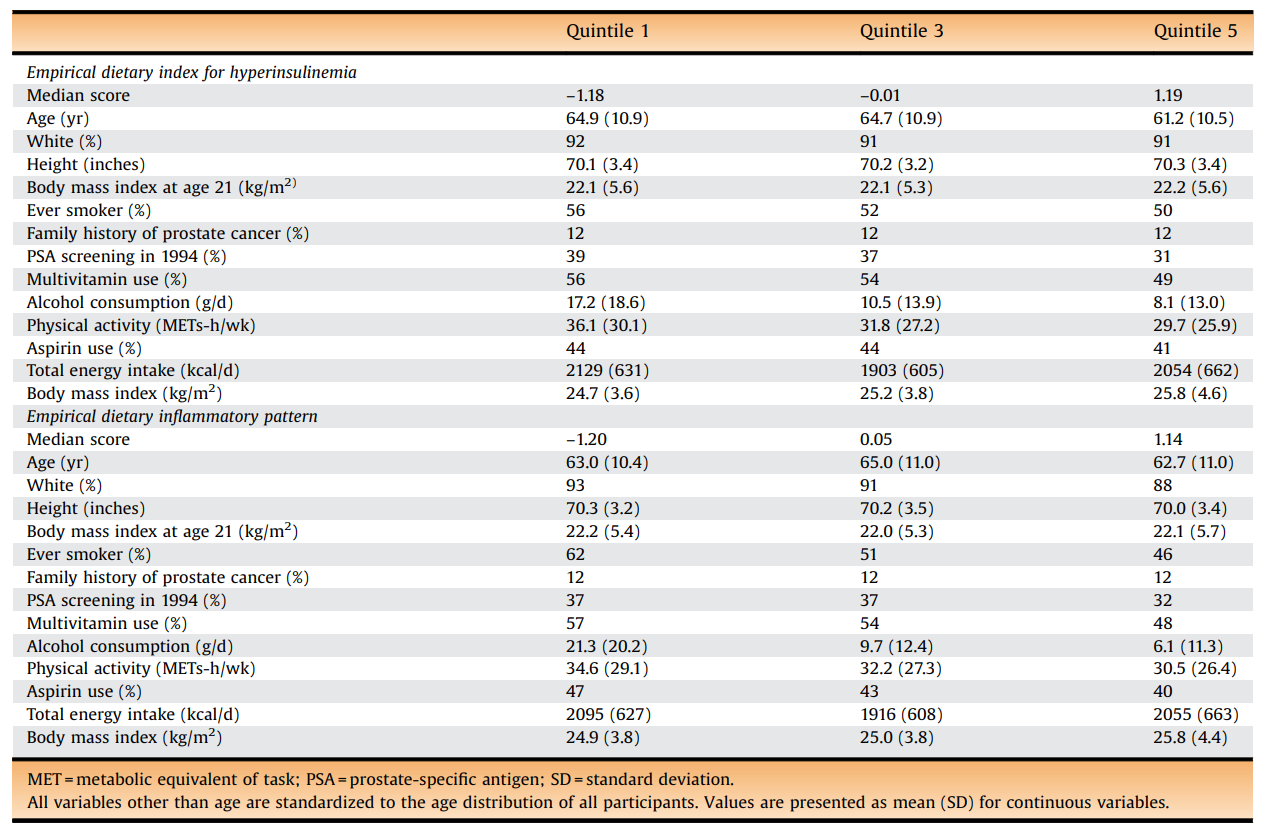
在健康专业人员随访研究(1986 - 2014)中,高胰岛素血症和炎症性饮食评分的参与者特征按人年的五分位数加权。
在28年的随访中,记录了5929例全前列腺癌,包括1019例晚期和667例死亡。在多变量校正模型中,高胰岛素饮食每增加一个标准差(SD),患晚期前列腺癌的风险增加7%(HR:1.07;95%CI:1.01 1.15),患致命性前列腺癌的风险增加9%(HR:1.09;95%CI:1.00 1.18)。当按年龄分层时,高胰岛素血症饮食仅与早发性侵袭性前列腺癌(65岁以下男性)相关,每SD HRs为1.20 (95% CI: 1.06 1.35)晚期,1.22(1.04 1.42)致命,1.20(1.04 1.38)致命。在整个研究人群中,炎症饮食与前列腺癌风险无关,但与早发致死性前列腺癌相关(每SD增加HR: 1.16;95%可信区间:1.00 1.35)。
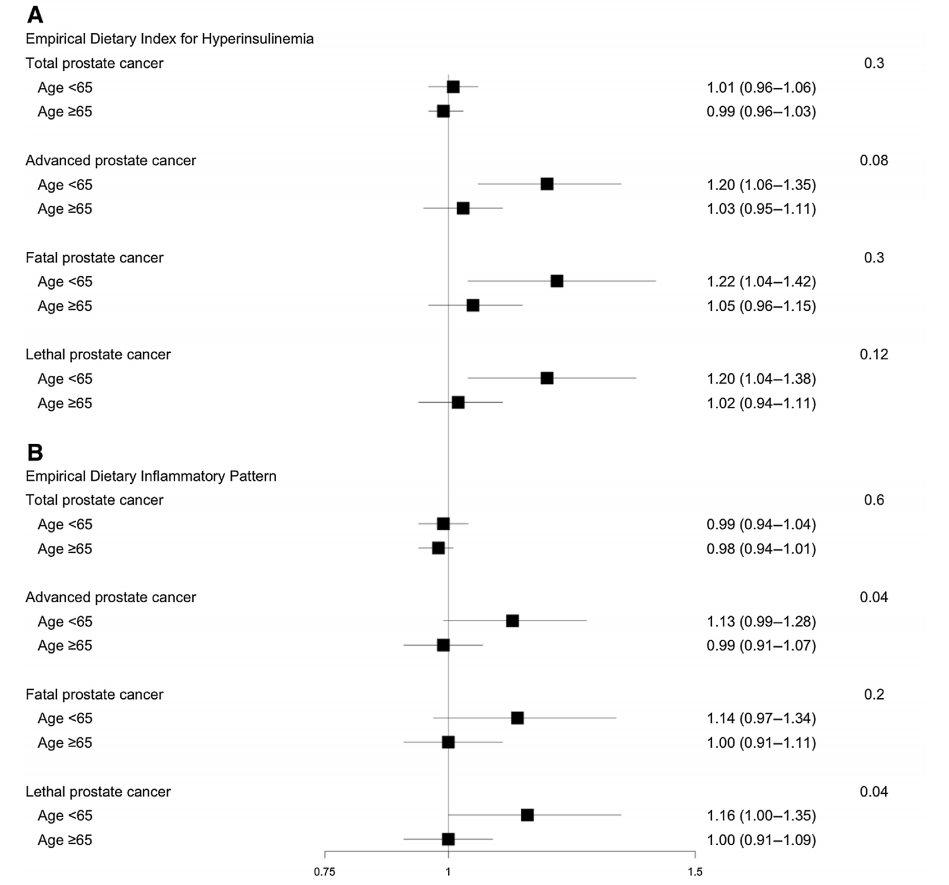
(A)高胰岛素血症和(B)炎性饮食与年龄亚组前列腺癌风险相关的多变量调整危险比和95%置信区间。
这项大型前瞻性队列研究的结果支持了以下假设:摄入具有较高胰岛素潜能的饮食与患侵袭性前列腺癌的风险更高相关。值得注意的是,即使在对BMI进行额外调整后,这些关联仍然存在,而且在最近的饮食习惯和年轻男性中往往更强。在整个研究人群中,促炎饮食与前列腺癌风险无关,但在65岁以下的男性中与致命性前列腺癌相关。
在本研究中使用的两种饮食类型包括许多在其他饮食模式中不典型的食物组,包括特定的蔬菜类别(如绿叶蔬菜)、咖啡和动物性食物,除了红肉和加工肉类,如鸡蛋。其中一些已经被证明在前列腺癌的背景下具有潜在的重要作用,特别是对于更具侵袭性的肿瘤。因此,不包括这些食物的饮食模式可能遗漏了影响前列腺癌风险的饮食关键方面,并可以部分解释先前的零发现。
尽管循环胰岛素或c肽与前列腺癌风险的病例对照研究的结果有些复杂,一些来自流行病学和实验研究的其他证据表明高胰岛素血症在前列腺癌中起作用。血清胰岛素与前列腺癌复发相关,而内科医生健康研究发现诊断前c肽可以预测前列腺癌死亡率。此外,代谢综合征与更高的前列腺癌风险相关,特别是具有更强侵袭性的肿瘤特征和生化复发,而且有报道称使用二甲双胍可以提高前列腺癌患者的生存率。
炎症的某些方面与高胰岛素血症密切相关,在本研究中,炎症通过高胰岛素血症和胰岛素抵抗对IGF轴的潜在作用可能有助于炎症性饮食与年轻男性中侵袭性前列腺癌之间的联系。许多研究报道了循环炎症生物标志物与前列腺癌风险之间的关系。炎症性饮食也可能通过组织水平炎症导致前列腺癌的病因,因为前列腺炎在中青年男性中特别常见,前列腺肿瘤活检中也经常观察到炎症。这一结论得到了前列腺组织性传播感染和感染源的流行病学研究的支持。
总之,高胰岛素血症和炎症可能是将饮食模式与侵袭性前列腺癌风险联系起来的潜在机制,特别是早发性疾病。
参考文献:Benjamin C. Fu,et al. Insulinemic and Inflammatory Dietary Patterns and Risk of 4 Prostate Cancer,European Urology January 06, 2021. DOI:https://doi.org/10.1016/j.eururo.2020.12.030
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#胰岛#
32
#PE#
42
学习了
83
#饮食模式#
46
#炎症性#
39
学到了很多
80
前列腺癌相关研究,学习了,谢谢梅斯
35