Clinical & Translational Immunology:紫外线晒伤后,我们的皮肤是如何自愈的?
2020-04-13 Walter 转化医学网
导言:尽管春天的阳光还不很毒辣,但口罩下的精致女人们已然是全套妆容外加厚厚一层防晒霜。诚然,多重防晒很有必要。阳光中的紫外线会对人体产生许多不利影响,例如诱发炎症、光皮病,严重情况下甚至导致皮肤的免疫
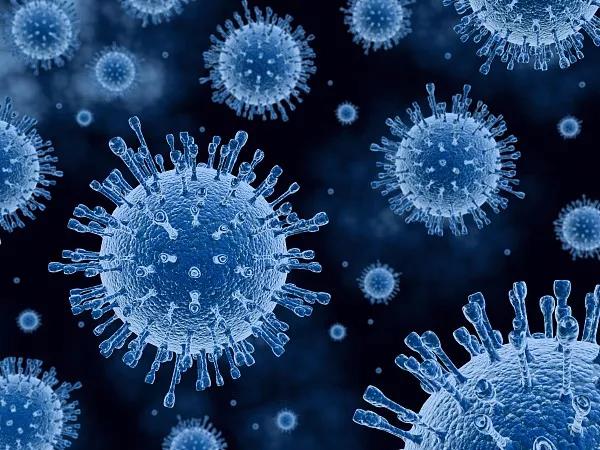
导言:尽管春天的阳光还不很毒辣,但口罩下的精致女人们已然是全套妆容外加厚厚一层防晒霜。诚然,多重防晒很有必要。阳光中的紫外线会对人体产生许多不利影响,例如诱发炎症、光皮病,严重情况下甚至导致皮肤的免疫抑制和皮肤癌。爱晒太阳的美国人,每年因皮肤癌产生的医疗咨询和治疗费用就高达数十亿美元。因此,解读紫外线如何调解皮肤免疫微环境,可能提示着防晒和修复的新途径。
英国曼彻斯特大学的Lesley Rhodes课题组近日在Clinical & Translational Immunology期刊上发表重要工作,发现人类皮肤在紫外线晒伤后,CD4+ GATA3+和CD8+ GATA3+两种T细胞被招募到皮肤表面,并进行长达14天以上的修复过程,提示靶向刺激这些免疫细胞可能预防并加速改善晒伤皮肤状况。

紫外线(UVR)辐射长时间暴露(约4-6小时),我们的皮肤会出现红斑、疼痛和水肿,这就是皮肤对紫外线损伤的自分解性炎症反应。发炎后,组织不会立即恢复稳态,取而代之的是发生“自适应稳态”;此时,尽管起始的炎症信号已经消退,继发性浸润或炎症消退后免疫细胞将保留,以维持免疫抑制环境。此前研究证明,调节性T细胞(Tregs)对于小鼠暴露于UVR后的皮肤免疫抑制至关重要,但人类皮肤如何自愈却尚未可知。
因此,研究者招募了一群健康的志愿者,在曼彻斯特大学Salford Royal的光生物学部门进行实验,将志愿者的某一部分皮肤安全地暴露于单一剂量的、足以引起炎症的UVR中;随采集皮肤样本,并用质谱等手段检测了皮肤成分和免疫情况随UVR暴露时间的变化。
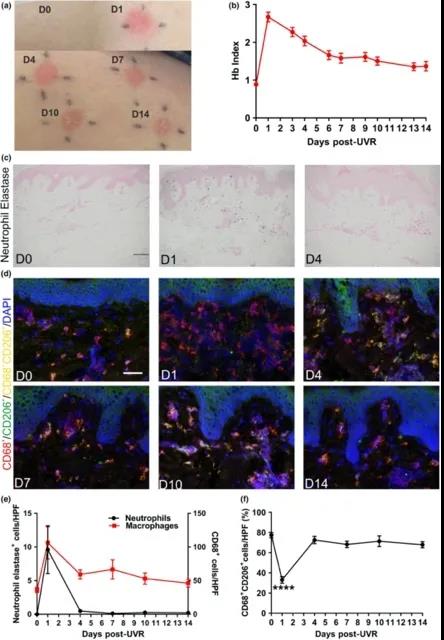
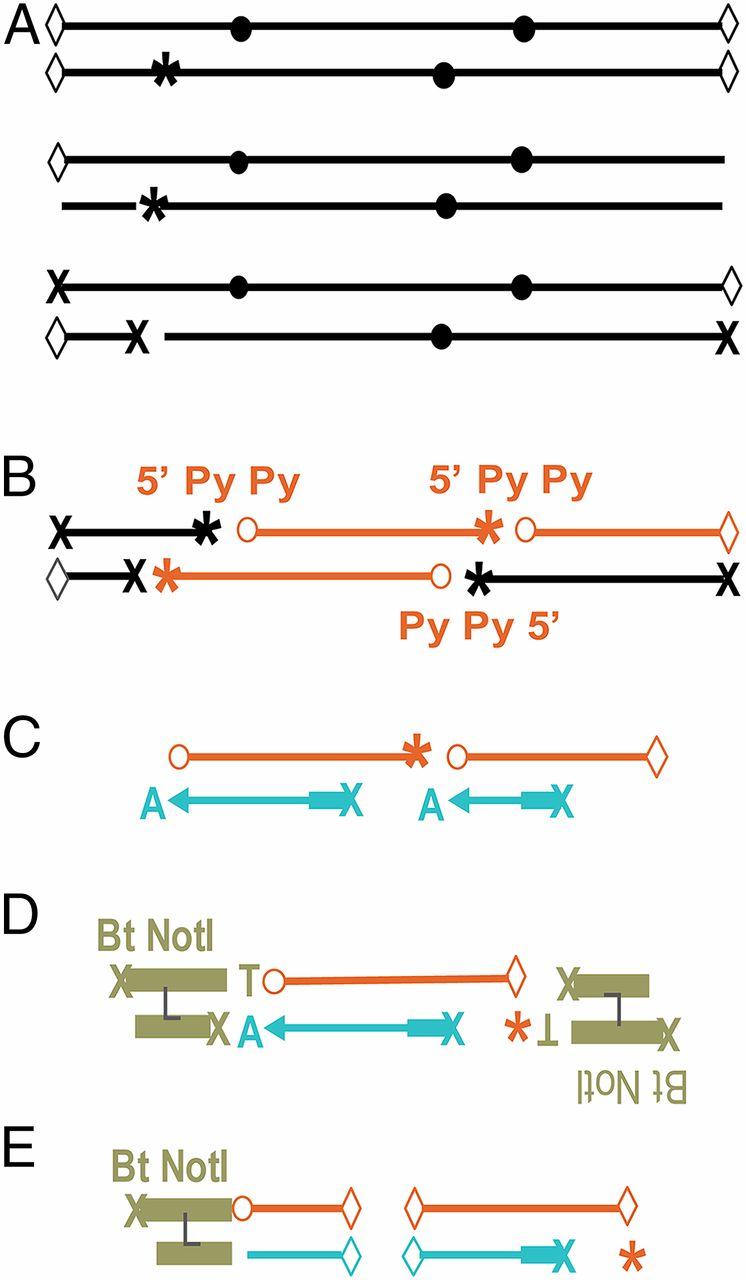
人类皮肤在UVR暴露后4天即发生细胞分解
结果显示,典型的细胞分解在UVR暴露4天后就会发生;14天内CD4+ GATA3+和CD8+ GATA3+两种T细胞被UVR引发的炎症招募并保留在人体皮肤的发炎区域,并改变皮肤成分,帮助皮肤在紫外线照射后自我修复。
这里,研究者在人类皮肤发现CD8+ GATA3+ T细胞与在小鼠模型中发现的CD4+Tregs不同,CD8+亚型细胞在炎症之后得以保留,研究者猜测其能通过促进GATA3表达,从而提高IL-10含量,以产生免疫抑制活性。换言之, UVR诱导的人类炎症还涉及“分解后阶段”,此时免疫调节作用保持在较高的水平,这意味着UVR暴露后免疫系统的自我稳定和修复。
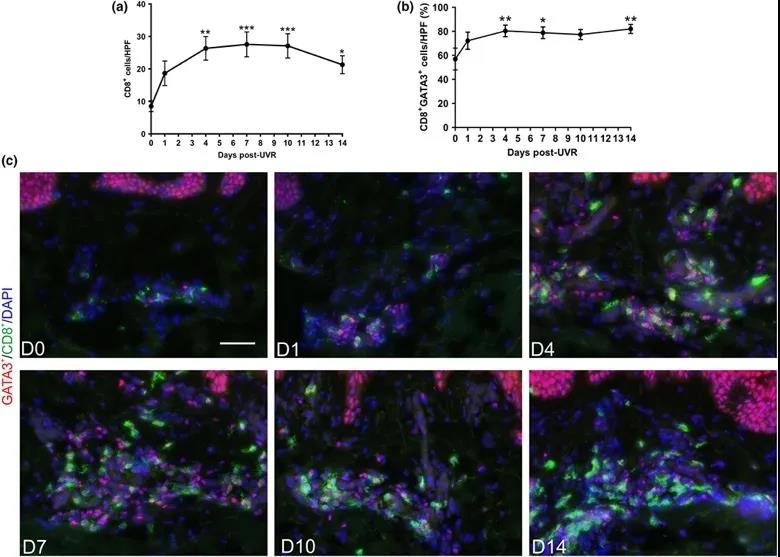
暴露14天内,UVR诱发的炎症招募并保留CD8+ GATA3+ T细胞
最后,研究者在UVR暴露后14天的人类皮肤中,依然检测到较高的免疫活性,说明炎性刺激后延长的免疫抑制状态有助于预防“适应性稳态”。具体而言,急性炎症后,前列腺素和羟基脂肪酸的合成增加,而CD8+ GATA3+ T细胞得以保留在皮肤中。
由于UVR暴露后会大量释放潜在的自身抗原,因此这些免疫细胞和介体可能是维持免疫抑制环境和预防慢性炎症或自身免疫所必需的。研究者认为,靶向提高这些免疫细胞(例如CD4+ / CD8+ GATA3+细胞)的活性以增加IL-10或M2MФs以及操纵脂质介体的合成,可加快炎症消退并改善UVR暴露导致细胞分解后的皮肤微环境。
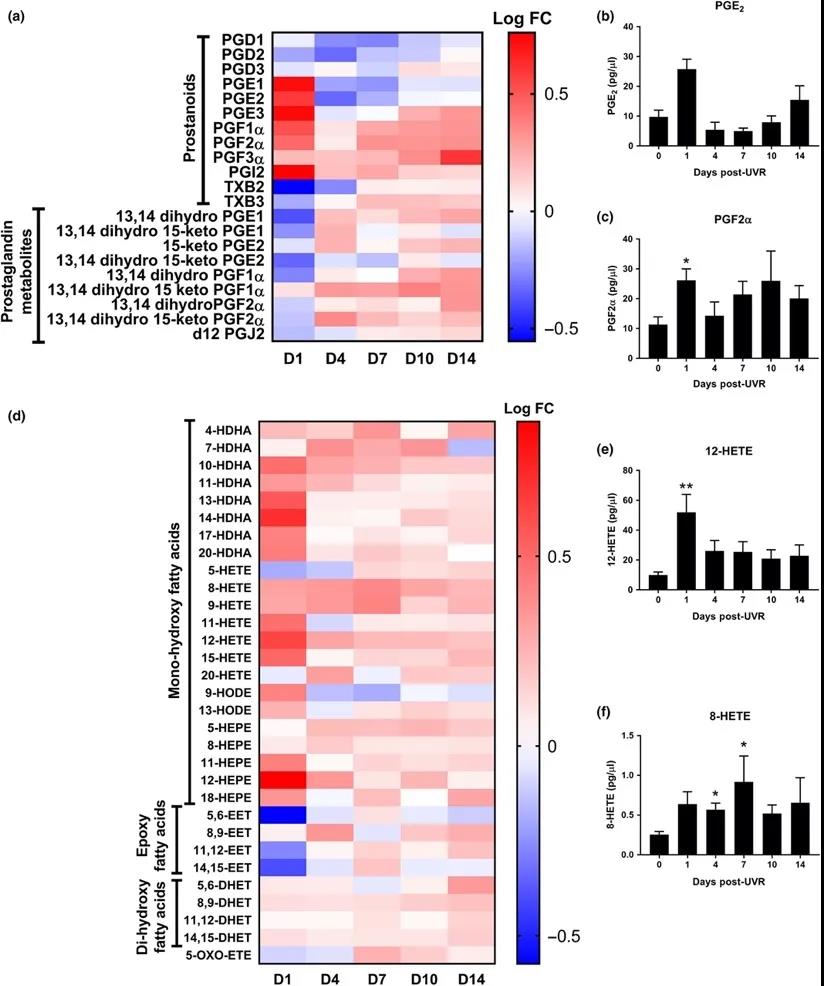
UVR暴露14天内,前列腺素和羟基脂肪酸的合成增加
Hawkshaw等人的研究结果揭示了一个有趣的现象,即在紫外线暴露后特定类型(CD4+ / CD8+ GATA3+)的免疫细胞将在皮肤表面保留一段时间,并参与皮肤自我防御和修复过程,这将是修复晒伤和预防皮肤癌的重要靶点;并且该结果突破了之前在小鼠模型中的发现,表明鼠类皮肤对UVR的反应无法合理外推到人类皮肤中,因此说明针对UVR的护肤品和药物还需经人体实验以检验其功效。
原始出处:
Nathan J Hawkshaw, Suzanne M Pilkington, Sharon A Murphy, et.al. UV radiation recruits CD4+GATA3+ and CD8+GATA3+ T cells while altering the lipid microenvironment following inflammatory resolution in human skin in vivo. Clinical & Translational Immunology 02 April 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#自愈#
40
#TRA#
36
#Transl#
32
#Translation#
34
#translational#
31
实用啊
83
#clinical#
28