Prostate:基线血清IL-8对转移激素敏感性前列腺癌结果的影响
2020-09-28 AlexYang MedSci原创
肿瘤细胞和一些骨髓细胞产生的免疫抑制性细胞因子白细胞介素-8(IL-8)能够促进炎症、血管生成和转移。在研究人员的探索过程中,雄激素剥夺疗法(ADT)起始时血清IL-8升高预示着更差的总生存(OS)。
肿瘤细胞和一些骨髓细胞产生的免疫抑制性细胞因子白细胞介素-8(IL-8)能够促进炎症、血管生成和转移。在研究人员的探索过程中,雄激素剥夺疗法(ADT)起始时血清IL-8升高预示着更差的总生存(OS)。最近,有研究人员利用ADT+/-多西他赛治疗转移性激素敏感性前列腺癌(mHSPC)患者的3期CHAARTED试验的血清样本,验证了上述发现。
研究人员在203名患者开始接受ADT治疗的28天内抽取了血清样本。研究结果发现,较高的IL-8水平对较短的OS(连续:HR 2.2,95%CI:1.4-3.6,P=0.001;二元>9.3:HR 1.7,95% CI:1.2-2.4,P=0. 007)和发展为CRPC的时间(连续:HR 2.3,95% CI:1.6-3.3,p<0.001;二元:HR 1.8,95% CI:1.3-2.5,p<0.001)具有预后作用,且与多西他赛的使用、疾病负担和转移时间无关。包括发现队列在内的Meta分析同时表明,单独使用ADT治疗的患者二元IL-8水平>9.3pg/ml,且对较差的OS(HR 1.8,95% CI:1.2-2.7,p=0 .007)和较短的CRPC时间(HR 1.4,95% CI:0.99-1.9,p=0.057)具有预后性。
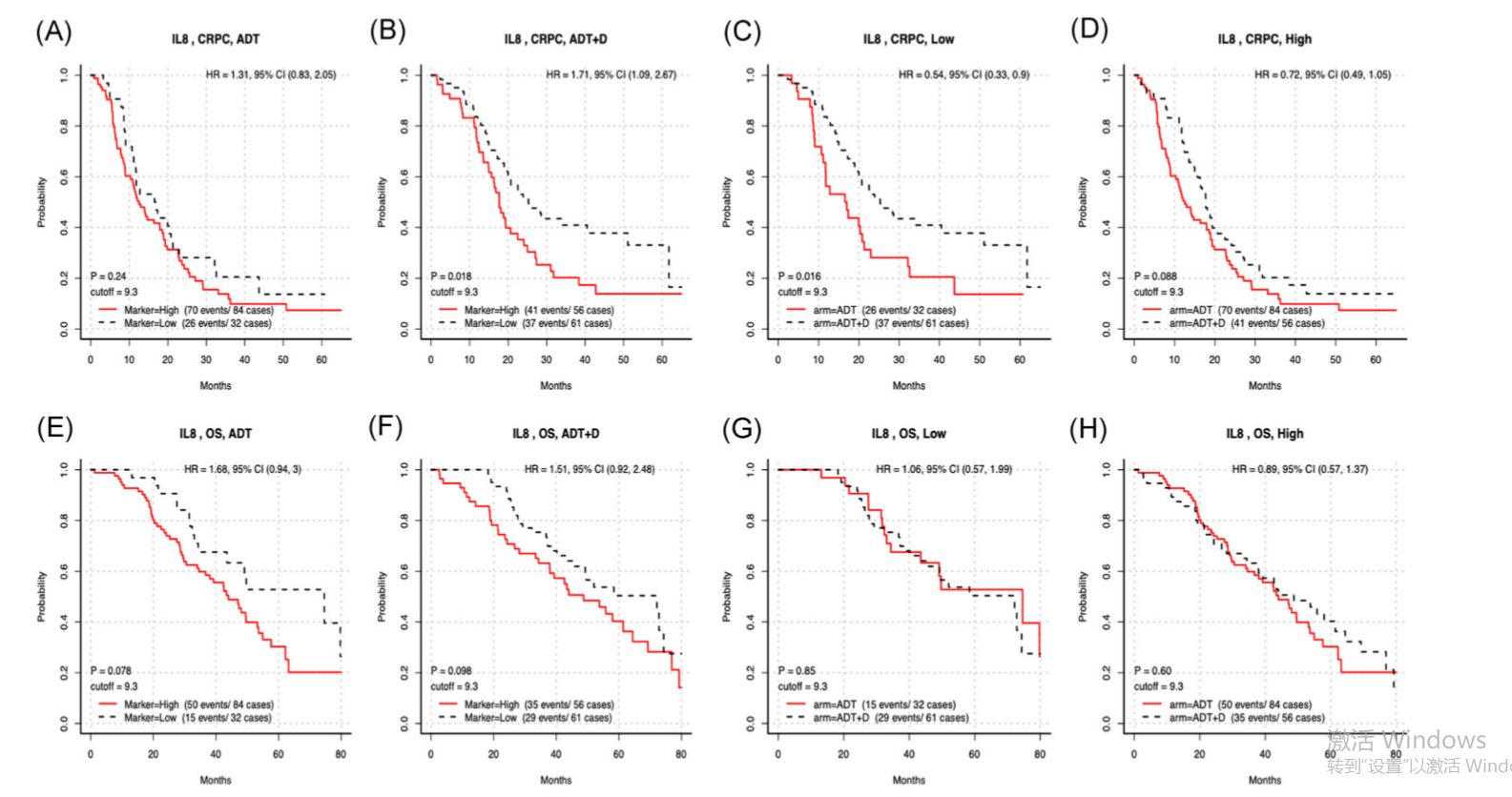
E3805队列中IL-8水平和结果的Kaplan–Meier曲线
最后,研究人员指出,在ADT起始治疗的患有mHSPC男性进行的3期CHAARTED研究中,IL-8的升高预示着更差的生存期和更短的发展为去势抵抗性前列腺癌时间,且与多西他赛的给药、转移性负担以及异时或新生转移性无关。他们的研究结果支持将IL-8作为改善mHSPC治疗结果的策略。
原始出处:
Lauren C Harshman , Victoria X Wang , Anis A Hamid et al. Impact of baseline serum IL-8 on metastatic hormone-sensitive prostate cancer outcomes in the Phase 3 CHAARTED trial (E3805). Prostate. 2020 Sep 19
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#ROS#
21
#敏感性#
31
#PRO#
30
#IL-8#
44
前列腺癌相关研究,学习了,谢谢梅斯
40