背景
患者在心脏手术后认知功能下降较为常见。现有文献对术中影响性因素或保护性因素的作用尚无定论。
方法
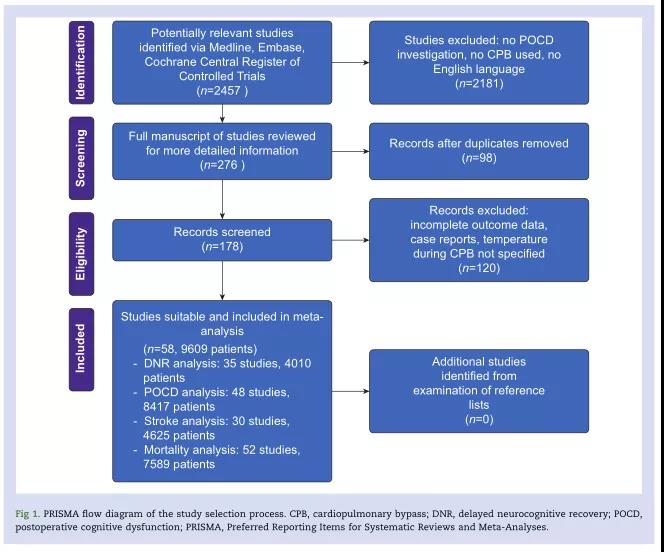
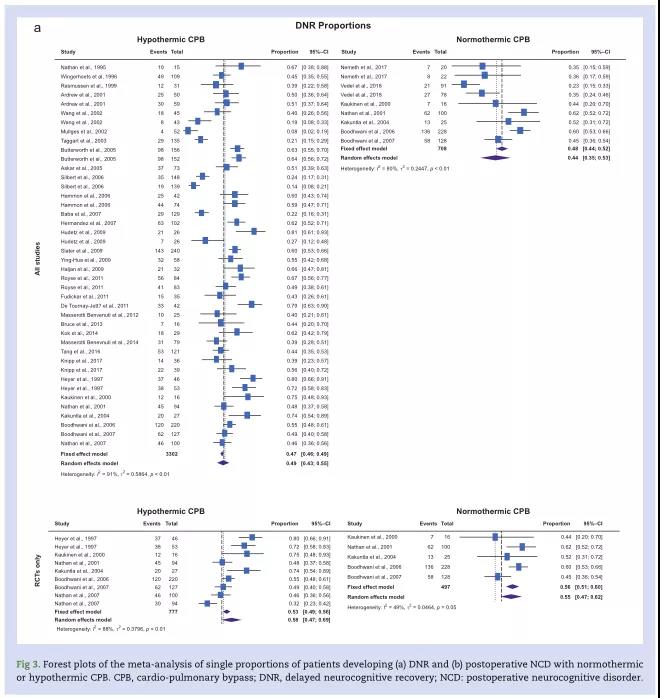
我们系统地回顾了评估低温或常温体外循环(CPB)患者神经认知延迟恢复(DNR)、术后神经认知障碍(NCD)、卒中和死亡率的研究。我们进一步对年龄、手术类型(冠状动脉旁路移植术[CABG]、瓣膜手术或联合手术)和CPB期间的平均动脉压(MAP)进行了亚组分析,并在计算了单一比例和置信区间(CI)后进行了比例Meta分析。
结果
我们的分析显示:在共纳入的58项研究、9609名患者中,4010例患者中有1906例(47.5%)发生了DNR,7160例患者中有2071例(28.9%)发生了NCD。4625名患者中90名(2.0%)发生卒中,7589名患者中174名(2.3%)死亡。所考虑的变量与DNR、NCD、卒中和死亡率之间没有统计学意义的关系。亚组分析中,与常温CPB相比,低温CPB下进行联合手术后的患者NCD发生率较高,在常温CPB下行联合手术后患者的DNR和NCD发生率低于CABG手术。与CPB期间MAP≤50~70 mmHg患者相比,CPB期间MAP>70 mmHg的患者DNR发生率较低。
结论
体外循环期间的体温、MAP和手术类型与心脏手术中的神经认知障碍、中风和死亡率无关。常温体外循环,尤其是在MAP>70 mmHg的情况下,可以降低心脏手术后神经认知功能下降的风险。
原始出处:
Federico Linassi, Eleonora Maran, Alessandro De Laurenzis, et al. Targeted temperature management in cardiac surgery: a systematic review and meta-analysis on postoperative cognitive outcomes[J]. Br J Anaesth, 128 (1): 11e25 (2022).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Meta#
58
#ANA#
32
#系统综述#
53
#EST#
38
#MET#
31