Ann Surg:肝移植可为不可切除性肝转移的结直肠癌患者提供较长的总生存期
2020-12-06 MedSci原创 MedSci原创
接受姑息性化疗的不可切除性结直肠癌患者5年总生存率约为10%。既往一项研究(SECA-I)中,肝移植为患者提供了60%的总生存率。死亡的危险因素是癌胚抗原(CEA)>80μg/L,化疗时病
接受姑息性化疗的不可切除性结直肠癌患者5年总生存率约为10%。既往一项研究(SECA-I)中,肝移植为患者提供了60%的总生存率。死亡的危险因素是癌胚抗原(CEA)>80μg/L,化疗时病情进展,最大病灶大小>5.5cm,从原发肿瘤切除到移植不到2年。本项前瞻性(SECA-II)研究旨在评估部分接受肝移植的不可切除的结直肠癌患者的总生存期和无病生存期,研究结果已在线发表于Ann Surg。

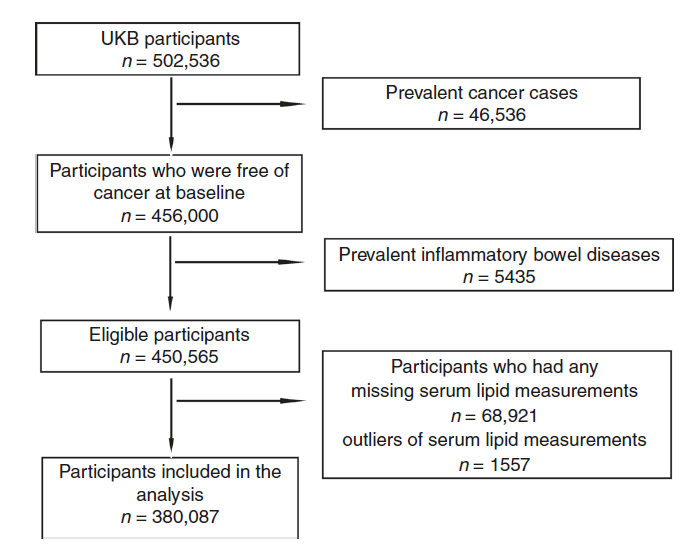
研究纳入了由计算机断层扫描(CT)/磁共振成像/正电子发射断层扫描确定的不可切除的仅肝脏转移的结直肠癌患者,并且对化疗至少有10%的反应。从诊断到肝移植的时间要求在1年以上。
结果显示,在中位随访36个月时,1年、3年和5年的Kaplan-Meier总生存率分别为100%、83%和83%。1、2、3年的无病生存率分别为53%、44%、35%。1、2、4年复发时的总生存率分别为100%、73%、73%。复发主要是生长缓慢的肺转移瘤,可进行治愈性切除。诊断时Fong临床风险评分为1~2分,无病生存期比3~4分长(P=0.044)。本研究纳入的患者预后因素明显优于之前的SECA-I研究。
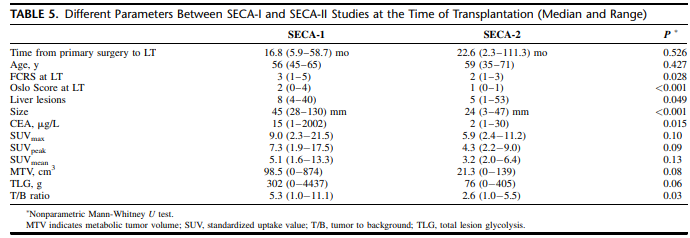
该研究结果表明,肝移植为不可切除性肝转移的结直肠癌患者提供了最长的总生存期。改良的选择标准使不可切除的结直肠癌肝转移患者的5年总生存期与其他肝移植适应症相当。
原始出处:
Svein Dueland, Trygve Syversveen, et al., Survival Following Liver Transplantation for Patients With Nonresectable Liver-only Colorectal Metastases. Ann Surg. 2020 Feb;271(2):212-218. doi: 10.1097/SLA.0000000000003404.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#生存期#
35
#肝转移#
0
#结直肠#
23
#总生存期#
28