BMC Gastroenterology: 术前血小板计可以预测肝移植患者移植后门静脉并发症概率
2021-01-21 MedSci原创 MedSci原创
肝移植被认为是晚期肝病患者的唯一治疗选择。在过去的几十年里,肝移植的效果已经随着外科技术的进步,免疫抑制的发展和围手术期护理完善获得大大改善。
肝移植被认为是晚期肝病患者的唯一治疗选择。在过去的几十年里,肝移植的效果已经随着外科技术的进步,免疫抑制的发展和围手术期护理完善获得大大改善。但是,肝移植后发病率仍然很高,这可能会影响患者的生存和生活质量。血小板是各种生理和病理过程的主要参与因素。最近的研究已经表明,血小板不仅在止血和组织修复中扮演重要角色,而且在肿瘤生长和转移,以及肝脏的再生中发挥作用。患有严重肝病的肝移植患者的血小板计数和功能受损。因此,本项研究旨在评估术前血小板计数对肝移植术后并发症发生率的影响。
研究人员对2015年1月至2018年9月间接受肝移植的患者的临床数据进行评估。在329名患者中,平均年龄为46.71±0.55岁,其中243名是男性(75.2%)。高血小板计数组(> 49.5×109 / L; n=167)移植后门静脉并发症的发生率明显高于低血小板计数组(≤49.5×109 / L,n = 162,12.6% VS 1.9%)。经过多变量回归分析后,高血小板计数与术后门静脉并发症独立相关(OR:8.821,95%置信区间[CI]:2.260-34.437)。经过治疗加权比重的反分析后,高血小板计数组的患者门静脉并发症的风险显着更高(OR:9.210,95%CI:1.907-44.498,p = 0.006)和同种异体移植早期功能障碍(OR:2.087,95%CI:1.131-3.853,p = 0.019)更加严重。
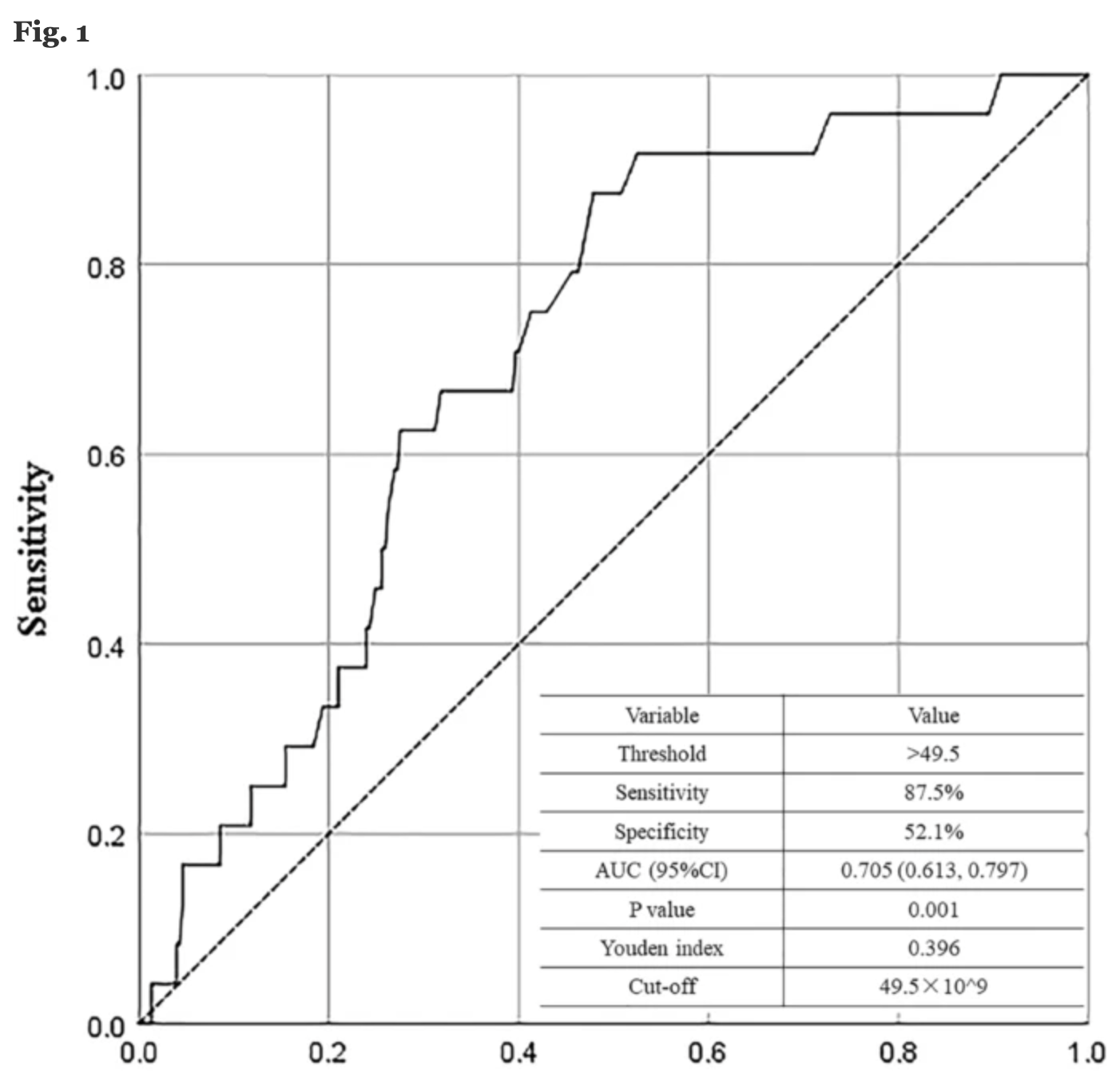
研究最后作者说道:术前血小板计数> 49.5×109 / L是移植后门静脉并发症和早期同种异体移植功能障碍的独立危险因素。术前血小板计数高可能是肝移植受者不良预后的指标。
原始出处:
Qingshan Li. Et al. Preoperative platelet count predicts posttransplant portal vein complications in orthotopic liver transplantation: a propensity score analysis. BMC Gastroenterology.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Gastroenterol#
38
#静脉#
43
#AST#
51
#GAS#
37
#并发#
42
#BMC#
31
#门静脉#
46
#Gastroenterology#
29
这个研究比较有新意
93