Aging Cell:淋巴瘤药物依鲁替尼可以缓解AD表型
2021-03-13 haibei MedSci原创
阿尔茨海默病(AD)是一种神经退行性疾病,发病后通常进展缓慢,逐渐恶化。尽管目前关于AD的研究众多,但AD的确切病理机制和有效的治疗策略仍不清楚。
阿尔茨海默病(AD)是一种神经退行性疾病,发病后通常进展缓慢,逐渐恶化。尽管目前关于AD的研究众多,但AD的确切病理机制和有效的治疗策略仍不清楚。
AD以两种神经病理症状为特征:淀粉样蛋白β(Aβ)斑块和神经纤维缠结(NFTs)。Aβ是由淀粉样β前体蛋白(APP)的蛋白分解加工产生的,Aβ的积累会损害记忆力,减少树突棘的形成,增加神经炎症和tau病。
在正常的单体形式下,蛋白tau在稳定微管方面起着重要作用。然而,在病理条件下,高磷酸化的tau从微管上脱落,被泛素化,并聚集成成对的螺旋纤维结构(PHFs)。PHFs可以造成神经毒性和突触NFTs,导致树突棘丢失、认知功能障碍,最后进展为神经退行性疾病。
尽管目前,Aβ和NFTs影响突触和认知功能的分子机制尚未完全阐明,但抑制和/或防止Aβ积累和tau的高磷酸化的药物可能对AD的靶向治疗有用。
已有的报道显示,细胞淋巴瘤药物依鲁替尼(ibrutinib)可以在体外和体内调节LPS诱导的神经炎症,但其对阿尔茨海默病(AD)病理和认知功能的影响尚未研究。最近,研究人员探究了依鲁替尼在两种AD小鼠模型中的影响。
在5xFAD小鼠中,注射依鲁替尼可以通过促进APP裂解的非淀粉样蛋白生成途径,显著降低Aβ斑块水平,减少Aβ诱导的神经炎症反应,并通过降低磷酸化环蛋白依赖性激酶-5(p-CDK5)的水平,显著下调tau的磷酸化。
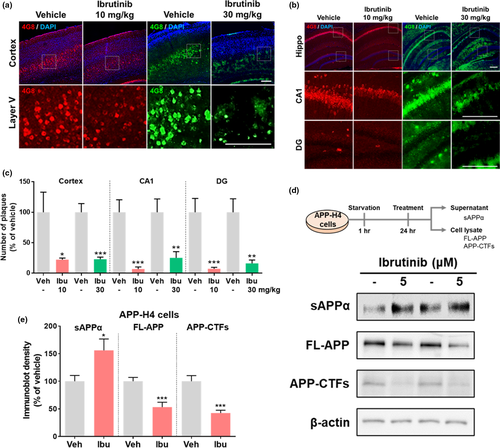
重要的是,在PS19小鼠中注射依鲁替尼也缓解了tau介导的神经炎症和tau磷酸化。
在5xFAD小鼠中,依鲁替尼改善了长期记忆和树突棘数量,而在PS19小鼠中,依鲁替尼没有改变短期和长期记忆,但促进了树突棘的生成。有趣的是,依鲁替尼对树突棘发生的诱导依赖于磷酸肌苷3-激酶(PI3K)的磷酸化。
总的来说,该研究结果表明,依鲁替尼可以调节AD相关病理和认知功能,可能是AD的潜在疗法。
原始出处:
Hyun‐ju Lee et al. Ibrutinib modulates Aβ/tau pathology, neuroinflammation, and cognitive function in mouse models of Alzheimer's disease. Aging Cell (2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Cell#
28
#CEL#
28
#表型#
26
棒
76
好文章!
69