Medicine :中国农村老年高血压患者血压应控制在140/90 mmHg以下还是150/90 mmHg以下?
2015-10-30 phylis 译 MedSci原创
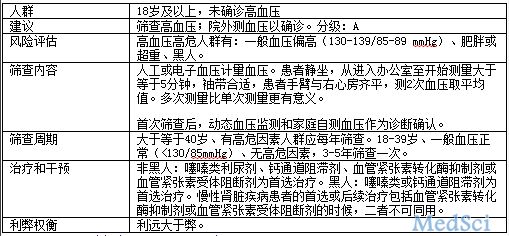
JNC-8最近推荐收缩压控制由最初的大于等于150 mmHg,大于60岁患者治疗目标应<150/90 mmHg。然而,一些随机对照试验机观察研究的结果不支持这个推荐。在这项前瞻性队列研究中,5006名中国农村高血压患者,年龄大于等于60岁。校正其他潜在的混杂因素,应用Cox比例风险模型评估随访平均的BP和预后(各种原因及心血管死亡,冠心病的发生及卒中)的相关性,随访时间中位数为4.8年。血
中国第八届全国委员会(JNC-8)最近推荐对于大于60岁高血压患者,当其血压超过150 mmHg的时候开始药物治疗,且血压治疗目标:其血压应控制在<150/90 mmHg。然而,一些随机对照试验机观察研究的结果不支持这个推荐。
在这项前瞻性队列研究中,5006名中国农村高血压患者,年龄大于等于60岁。校正其他潜在的混杂因素,应用Cox比例风险模型评估随访平均的BP和预后(各种原因及心血管死亡、冠心病的发生及卒中)的相关性,随访时间中位数为4.8年。血压(收缩压或舒张压)与不良预后呈上升或J型相关。与血压<140/90 mmHg相比,血压在140-149/<90 mmHg。患者各种原因的死亡率(HR: 2.698; 95% CI: 1.989-3.659),心血管死亡(HR: 2.702; 95% CI: 1.855-3.935),冠心病的发生(HR: 3.263; 95% CI: 2.063-5.161)及卒中(HR: 2.334; 95% CI: 1.559-3.945)显著升高。
老年高血压(140-149/<90 mmHg)患者发生不良预后的风险增加,提示基于JNC-8指南推荐血压控制在140-149/<90 mmHg对中国农村年龄大于60岁的高血压患者可能是不适合的。
原文出处:
Zheng L, Li J, Sun Z, et al. Relationship of Blood Pressure With Mortality and Cardiovascular Events Among Hypertensive Patients aged ≥60 years in Rural Areas of China: A Strobe-Compliant Study. Medicine (Baltimore). 2015,Sep.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#CIN#
37
#DIC#
34
#农村#
31
#高血压患者#
40
#老年高血压#
32
#Medicine#
28
#Med#
32
赞
134