Alz Res Therapy: 脑脊液中有哪些蛋白质,和tau-Aβ相关
2021-11-12 Freeman MedSci原创
跨膜蛋白与AD中淀粉样蛋白和tau等CSF标记物相关。
了解神经退行性疾病(如阿尔茨海默病(AD))的分子变化的演变,对于识别和验证用于诊断、预后或治疗的潜在生物标志物至关重要。除了AD的标志、淀粉样蛋白和tau病理学之外,与AD有关的一些早期变化已经被确认,如新陈代谢低下和脑内结构变化。
此外,大量的努力被用来确定脑脊液(CSF)蛋白质组的早期变化,以补充淀粉样β(Aβ42)、总tau(t-tau)和磷酸tau(p-tau)的测量。比如,神经丝轻链(NfL)已被认为是神经变性的标志物,可能被用来追踪AD的进展。
然而,除AD外,NfL在许多神经退行性疾病的CSF中也有增加,如额颞叶痴呆症、帕金森病和肌萎缩侧索硬化症。Neurogranin(NRGN)和neuromodulin(GAP43)是两个突触蛋白,据报道也与AD密切相关,但与NfL相比,它们似乎更具有疾病特异性。这两种蛋白在疾病发生前都显示出水平的改变,并与tau的CSF病理相关。
突触缺失和突触蛋白水平的改变发生在AD病程的早期,在轻度认知障碍(MCI)患者中已经可以检测到。神经变性或神经元死亡不足以解释突触的大量丧失,有人提出突触在神经元死亡前被选择性地去除。除了NRGN和GAP43外,一些突触蛋白在AD发病前也被发现有改变。
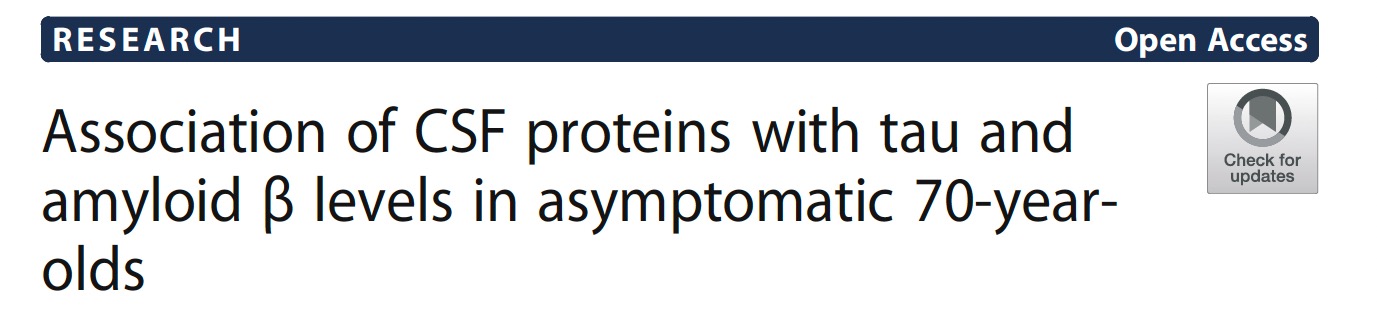
在认知能力正常和受损的老年人群中,发现了22种蛋白质在具有AD生物标志物特征的个体中的水平改变,这是由CSF的Aβ42、tau和p-tau水平定义的。在790个量化的蛋白质中,有59个与Aβ42、t-tau或p-tau的CSF病理学有关。在这59个蛋白质中,约有一半根据人类蛋白质图谱被分类为脑富集或脑升高。
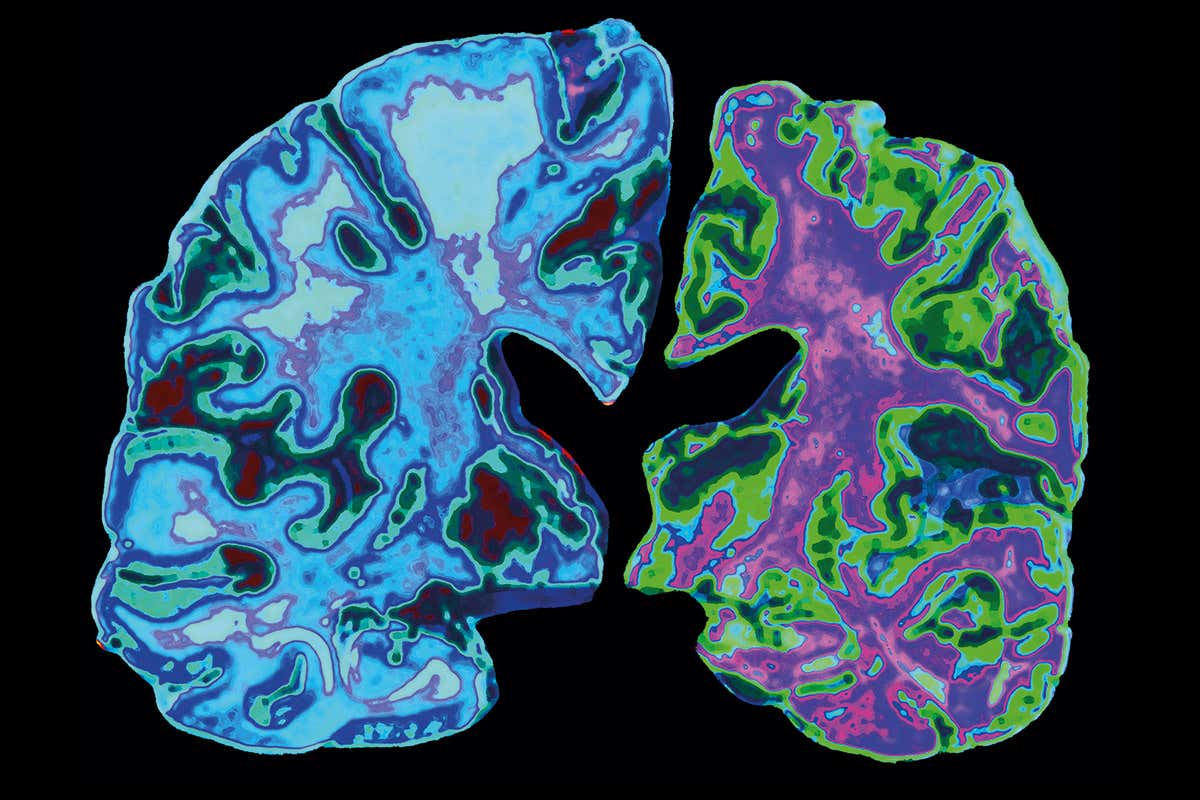
藉此,瑞典皇家理工学院的Julia Remnestål等人探究了104个蛋白质的关联,这些蛋白质已知是大脑富集的或与不同类型的神经退行性疾病有关,与CSF生物标志物的AD病理证据有关。
使用亲和蛋白质组学方法,他们对H70哥德堡出生队列研究(H70研究)中307名无症状70岁老人的CSF中的蛋白质水平进行了探索。H70研究是多学科的流行病学研究,研究了代表瑞典哥德堡老年人群的出生队列。
他们使用基于多重抗体和磁珠的技术探究了H70哥德堡出生队列研究中307名无症状70岁老人的脑脊液(CSF)中104种蛋白质的水平。
他们发现:蛋白水平首先与所有个体的总tau、phospho-tau和淀粉样β(Aβ42)的核心AD CSF生物标志物浓度相关。
63种蛋白质与总tau、磷酸tau或Aβ42显示出显著的相关性。
根据CSF Aβ42/Aβ40比率和临床痴呆评分(CDR)对个体进行划分,以确定病理和认知的早期变化是否对相关关系有影响。
他们还比较了各组之间分析的蛋白质与CSF标记物的关联,发现有33个蛋白质在淀粉样蛋白阳性个体和淀粉样蛋白阴性个体中显示出明显不同的关联,这是由CSF Aβ42/Aβ40比率决定的。按CDR评分划分的个体在关联方面没有差异。
这个研究的重要意义在于发现了一系列跨膜蛋白(与质膜相关、锚定在质膜上的蛋白、参与突触囊泡运输),他们与AD中淀粉样蛋白和tau等CSF标记物相关。
原文出处:
Remnestål J, Bergström S, Olofsson J, et al. Association of CSF proteins with tau and amyloid β levels in asymptomatic 70-year-olds. Alz Res Therapy. 2021;13(1):54. doi:10.1186/s13195-021-00789-5
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#白质#
32
#ERA#
25
#蛋白质#
29
#Tau#
33
#Aβ#
67