European Radiology:长期高强度降脂对老年人冠状动脉斑块的进展究竟有何影响?
2022-06-20 shaosai MedSci原创
近年来,冠状动脉计算机断层扫描(CCTA)的进步使得冠状动脉粥样硬化的无创评估与有创测量相比具有较高的诊断性能。
众所周知,心血管疾病仍然是全世界死亡和发病的主要原因。低密度脂蛋白胆固醇(LDL-C)在动脉粥样硬化性冠状动脉疾病(CAD)的进展中起着重要作用。
最近,一些研究通过血管造影和血管内超声(IVUS)成像显示,严格控制LDL-C水平可以防止冠状动脉疾病的进展,甚至促进动脉粥样硬化的消退。然而新的证据显示,强化降脂会诱发冠状动脉斑块钙化,从而加重冠状动脉钙化。同时,一些研究认为,虽然他汀类药物可能诱发冠状动脉斑块钙化,但这种发展可能只是正常疾病发展的一部分,而不是他汀类药物的影响。然而,冠状动脉钙化是主要不良心脏事件(MACEs)最有力的预测因素之一。因此,仍需进一步研究降低LDL-C对冠状动脉钙化的长期影响以及随年龄增长的表型转化。
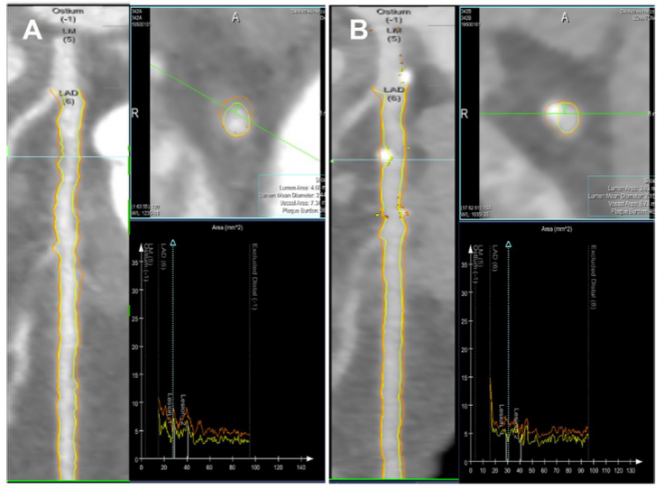
冠状动脉斑块的介入性成像评估主要是基于冠状动脉造影(CAG)、IVUS、光学相干成像(OCT)和其他技术。然而这些方法都是侵入性的且成本很高,因此不适合用于常规的临床筛查。此外,侵入性成像技术通常侧重于局部斑块负担的评估,但很难评估冠状动脉血管树的全长。近年来,冠状动脉计算机断层扫描(CCTA)的进步使得冠状动脉粥样硬化的无创评估与有创测量相比具有较高的诊断性能。半自动斑块分析软件能够准确、可重复地定量测量冠状动脉斑块体积,观察者之间和观察者内部的变异性低,因此可用于评估斑块负担和斑块成分随时间的变化。
近日,发表在European Radiology杂志的一项研究探讨了强化降低LDL-C对CCTA队列中斑块进展和钙化的长期影响,并评估了整个冠状动脉树冠状动脉硬化的变化,为冠心病患者的规范化治疗提供了参考。
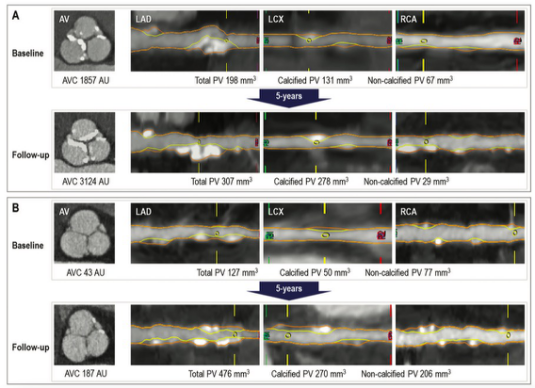
本项为期5年的队列研究共纳入了240名60岁以上的患者(包括754个病灶),每位患者均接受了连续的CCTA检查。患者被分为三组:强化降脂组、降脂组和对照组。对狭窄严重程度、斑块体积(PV)、斑块组成、PCPV和高危斑块(HRP)的存在进行了定量分析。在基线和随访时计算了CACS。
所有患者均为男性,平均年龄为66.8±5.8岁。随着时间的推移,观察到阻塞性冠状动脉病变的百分比增加(P < 0.001)。与基线时相比,梗阻性病变的百分比保持不变(p = 0.077),在随访的CCTA扫描中,强化降脂组的斑点状钙化百分比明显下降(p < 0.05)。强化降脂组的患者在钙化的PV、CACS和PCPV方面表现出更高的进展(所有P < 0.05),在纤维脂肪和富含脂质的PV方面表现出明显的衰减(所有P < 0.05),并高于其他组的患者。
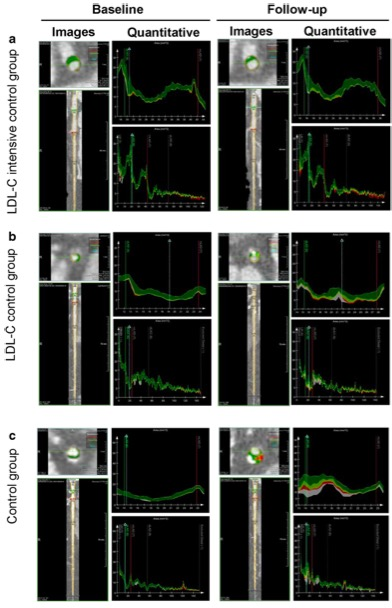
图 降LDL-C治疗对总斑块体积(PV)及其组成部分的长期影响。不同组别基线和随访的代表性CCTA图像(a, b, c)。CCTA,冠状动脉计算机断层扫描血管成像
本研究发现,在老年稳定型心绞痛队列中,即使接受了降低LDL-C的治疗,冠状动脉粥样硬化的总斑块体积也随着年龄的增长而增加。强化降低LDL-C与减少狭窄严重程度的发展和高危斑块特征有关。LDL-C强化控制组的患者表现出纤维脂肪和富含脂质的斑块体积明显减少,钙化进展。通过CCTA进行全面的系列斑块评估,将有助于进一步完善老年患者的风险分层和合理降脂治疗。
原文出处:
Ting Sun,Yabin Wang,Xinjiang Wang,et al.Effect of long-term intensive cholesterol control on the plaque progression in elderly based on CTA cohort study.DOI:10.1007/s00330-022-08594-w.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#冠状动脉斑块#
39
#PE#
37
#斑块#
37
#高强度#
46
学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习
49