Eur J Cancer:使用派姆单抗治疗的晚期黑色素瘤患者的长期结局
2021-10-01 Nebula MedSci原创
大部分采用派姆单抗治疗的早期(12周)病情稳定的黑色素瘤患者随后可获得部分或完全缓解
虽然当今社会对黑色素瘤风险因素的教育和认识均有所提高,但每年新确诊的病例数仍在持续增加。从历史上看,晚期黑色素瘤患者的预后很差,但随着靶向治疗和免疫检查点抑制剂的引入,这类患者的生存率得到了显著提高。
但早期病情稳定的黑色素瘤患者采用派姆单抗治疗的预后仍不明确。本研究旨在分析早期病情稳定的经治疗获得完全或部分缓解的黑色素瘤患者采用派姆单抗治疗的长期预后结果。
纳入了参与KEYNOTE-001和KEYNOTE-006研究并在第12周或第24周时病情稳定或获得部分/完全缓解的患者。
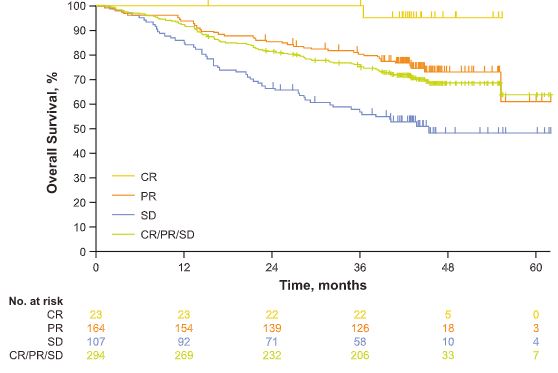
根据12周治疗反应分组进行的生存分析
在第12周分析纳入的294位患者中,有107位的病情稳定,其中7位(6.5%)获得了完全缓解,43位(40.2%)获得了部分缓解。第12周时完全缓解、部分缓解和病情稳定的患者48个月时的总生存(OS)率分别是95.2%、73.0%和47.7%。
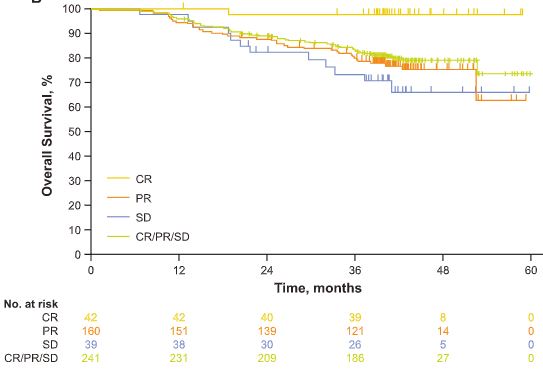
根据24周治疗反应分组进行的生存分析
第24周分析时,在241位患者中观察到了相似的结果。第12周病情稳定随后获得缓解的患者的48个月OS率为72.1%,第12周获得部分缓解且随后无变化的患者的48个月OS率为75.0%。第12周时病情稳定随后在第24周前病情进展的患者的36个月OS率和48个月OS率分别是11.6%和未达到。
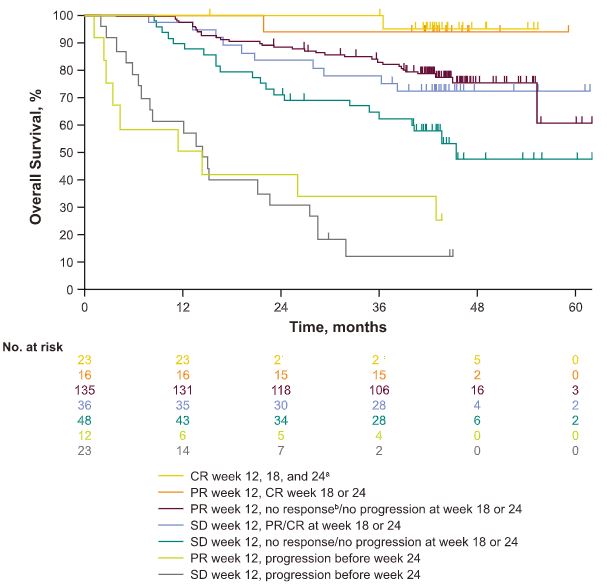
根据综合治疗反应变化进行的分析
综上所述,大部分采用派姆单抗治疗的早期(12周)病情稳定的黑色素瘤患者随后可获得部分或完全缓解。第12周时病情稳定并随后获得缓解的患者的存活预后与持续维持部分缓解的患者的相近。相反,12周时病情稳定但随后发生病情进展的患者的预后较差。该研究结果或可为早期获得病情稳定的患者的治疗决策提供指导。
原始出处:
Hamid Omid,Robert Caroline,Daud Adil et al. Long-term outcomes in patients with advanced melanoma who had initial stable disease with pembrolizumab in KEYNOTE-001 and KEYNOTE-006.[J] .Eur J Cancer, 2021, 157: 391-402. https://doi.org/10.1016/j.ejca.2021.08.013
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#色素#
35
#派姆单抗#
39
#长期结局#
32
#黑色素#
36
#黑色素#
38