Clin Cancer Res:Hedgehog信号抑制可改变胰腺癌微环境的成纤维细胞组成和免疫细胞浸润
2021-02-19 MedSci原创 MedSci原创
在胰腺癌中,Hedgehog信号到底是促进肿瘤生长还是抑制肿瘤生长?
胰腺导管腺癌(PDAC)是一种致命性疾病,以广泛纤维炎症间质为特征,含有丰富的癌症相关成纤维细胞(CAF)。PDAC的CAF具有异质性,但这种异质性的本质目前还未完全清楚。
Hedgehog通路在PDAC中以旁分泌方式发挥作用,癌细胞分泌的配体向微环境中的基质细胞发出信号。既往研究Hedgehog信号在PDAC中的作用的报道一直存在相互矛盾——既有研究报告Hedgehog信号可促进肿瘤生长,也有研究报告其可限制肿瘤生长。鉴于新发现的CAF异质性,Steele等人研究了Hedgehog通路抑制是如何重编程PDAC微环境的。
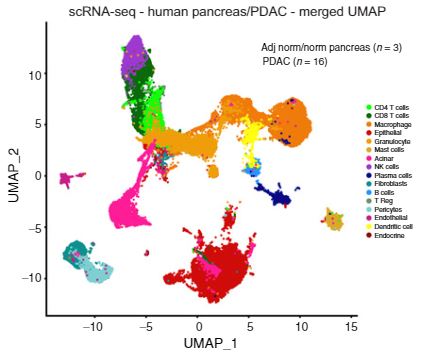
研究人员结合了药理抑制、功能获得性和功能丧失性遗传学实验、实时细胞计数和单细胞RNA测序来研究Hedgehog信号在PDAC中的作用。
研究人员发现,Hedgehog信号在成纤维细胞中被独特地激活,且在肌成纤维细胞性CAF(myCAF)和炎症性CAF(iCAF)中差异性高表达。Sonic Hedgehog过表达可促进肿瘤生长,但通过平滑的拮抗剂LDE225抑制Hedgehog通路会影响肿瘤生长。
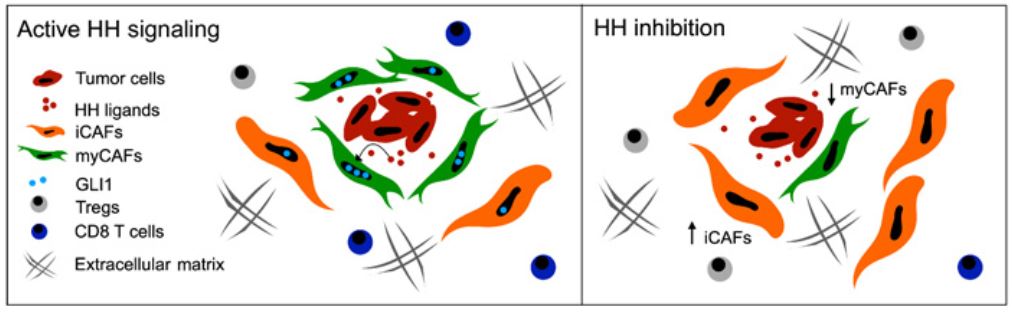
此外,Hedgehog通路抑制会减少myCAF的数量,增加iCAF的数量,这一点与细胞毒性T细胞的减少和调节性T细胞的扩增有关,还与免疫抑制相一致。
综上所述,Hedgehog通路抑制改变了胰腺癌微环境中成纤维细胞的组成和免疫细胞浸润。
原始出处:
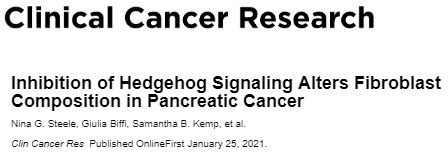
Steele Nina G,Biffi Giulia,Kemp Samantha B et al. Inhibition of Hedgehog Signaling Alters Fibroblast Composition in Pancreatic Cancer. Clin Cancer Res, 2021, 10.1158/1078-0432.CCR-20-3715
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Hedgehog#
31
#成纤维细胞#
37
#纤维细胞#
43