Diabetologia:少坐可以改善绝经后女性的代谢健康
2021-09-15 MedSci原创 MedSci原创
在当今社会,大多数人的久坐行为占主导地位,并与患2型糖尿病的风险有关。运动是有效预防和治疗2型糖尿病的基石,但在欧洲和美国的成年人中,维持积极的生活方式并定期进行中等到高强度的体育活动的依从性很低。
在当今社会,大多数人的久坐行为占主导地位,并与患2型糖尿病的风险有关。运动是有效预防和治疗2型糖尿病的基石,但在欧洲和美国的成年人中,维持积极的生活方式并定期进行中等到高强度的体育活动的依从性很低。有研究报道,用站立和步行来取代坐着的时间对2型糖尿病患者是有益的,但其潜在机制尚不清楚,也缺乏与运动的直接比较。
最近发表在Diabetologia的一篇文章直接比较了少坐或运动相对于久坐的代谢反应。
实验方法
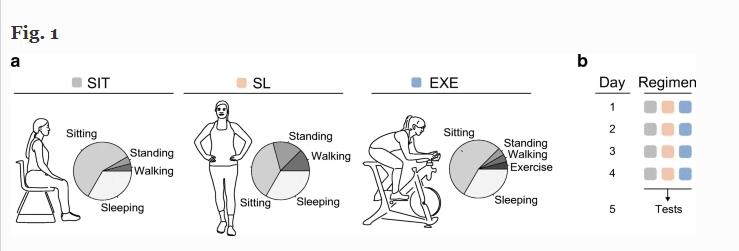
本研究对12名超重女性进行了一项随机、交叉干预研究,她们采用了三种良好控制的4天活动方案:(1)坐姿方案(静坐14小时/天);(2)运动方案(静坐13小时/天,运动1小时/天);(3)少坐方案(坐9小时/天,站立4小时/天,步行3小时/天)。主要结果是通过两步高胰岛素血症-低血糖钳夹测量胰岛素敏感性。此外,我们还对钳夹前的肌肉活检进行了代谢组学检测,以确定分子水平的变化。
Figure 1:实验方案如下图:
注:SIT:久坐方案;SL:少坐方案;EXE:运动方案
实验结果
用站立和步行代替坐着的时间超过4天,可以改善外周胰岛素敏感性,且与中度到剧烈运动的改善效果相当。与坐着的方案相比,少坐(~13%)和运动方案(~20%)的外周胰岛素敏感性有显著改善。此外,与坐着方案相比,少坐会使潜在的肌肉代谢组向中度至剧烈运动的方向移动。
Figure 2:少坐和运动方案比久坐方案提高胰岛素敏感性
a:高胰岛素输注率期间的血糖Rd,反映了外周(主要是肌肉)胰岛素敏感性,少坐和运动组显著较高;
b:少坐和运动组NOGD(非氧化葡萄糖清除)显著较高;
c:低胰岛素期的EGP(内源性葡萄糖产生)抑制,反映了肝脏胰岛素敏感性,在三种活动方案中相似;
d:MRS测定的IHL不受活动方案的影响。
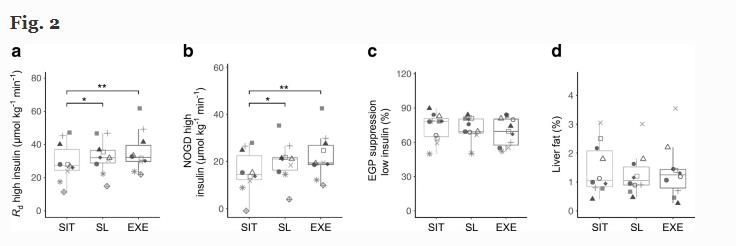
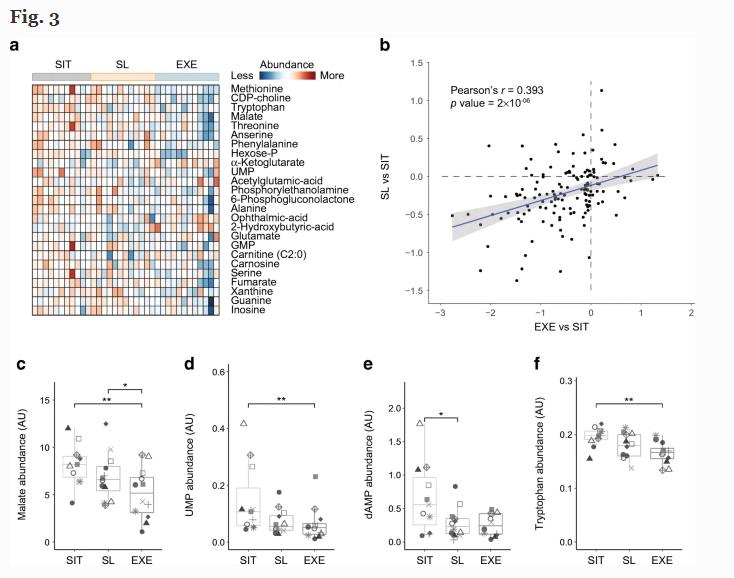
Figure 3:少坐会在分子水平上引起代谢变化,类似于运动引起的变化
a:前25种代谢物的热图
b:少坐引起的代谢变化和运动引起的代谢变化呈显著正相关
c-f:从久坐到少坐再到锻炼;例如苹果酸,尿苷酸,脱氧腺苷一磷酸,色氨酸,蛋氨酸和苏氨酸等代谢物的丰度呈阶梯式下降。
结论
用轻微的体育活动,如站立和行走,取代久坐的时间,可以有效地改善外周胰岛素敏感性。在骨骼肌中,运动和少坐疗法揭示了类似的胰岛素敏感性生理效应和类似的潜在分子代谢变化。因此,在改善代谢健康方面,相比于中度到剧烈的运动,通过站立和步行来持续替代坐着的时间可能是一个有吸引力的、更可行的选择。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#DIA#
34
#BET#
35
站着比坐着好,坐着比躺着好。
67
#绝经#
31
#绝经后女性#
48
#代谢健康#
33
#绝经后#
36