AJTR:多靶点治疗复杂性狼疮性肾炎临床分析
2022-03-21 从医路漫漫 MedSci原创
系统性红斑狼疮(SLE)是一种自身免疫性疾病,由其引起的最常见和最严重的器官损害是狼疮性肾炎(LN)。III型+V型或IV型+V型LN的治疗特别困难,通常被称为复合型LN。
背景:系统性红斑狼疮(SLE)是一种自身免疫性疾病,由其引起的最常见和最严重的器官损害是狼疮性肾炎(LN)。III型+V型或IV型+V型LN的治疗特别困难,通常被称为复合型LN。对于III+V型或IV+V型LN患者的治疗方法存在争议。据报道,目前推荐的治疗LN的方法是美国国立卫生研究院(NIH)的方法,该方法将糖皮质激素和环磷酰胺(CYC)静脉注射相结合。然而,临床上仍然存在较高的无效率和较高的复发率。部分患者预后差,停药后易复发,尤其是复杂性LN。此外,环磷酰胺可诱发或加重感染,引起性腺损害、白细胞减少、肝脏损害等副作用,限制了其应用。他克莫司(FK506)可以抑制IL-2和IL-10的产生,从而抑制T淋巴细胞和B淋巴细胞的增殖,在治疗狼疮性肾炎方面显示出良好的疗效。霉酚酸酯(MMF)选择性地阻断T和B淋巴细胞的增殖并抑制抗体的合成以达到免疫抑制的效果。先前的一项研究报告称,多靶点(他克莫司+霉酚松+泼尼松)治疗复杂性LN具有较高的短期缓解率和良好的安全性。然而,关于多靶点治疗的长期观察研究很少。本文报告了多靶点治疗复杂性狼疮性肾炎的疗效,并对其进行了长达72周的观察。
目的:观察多靶点(他克莫司+霉酚酸酯+泼尼松)治疗III型+V型和IV型+V型狼疮性肾炎的疗效和安全性。
方法:将56例狼疮性肾炎患者随机分为多靶点治疗组和环磷酰胺联合强的松治疗对照组,每组28例。观察治疗前、治疗后4、12、24、48、72周的临床指标及不良反应。
结果:1例患者在治疗72周内因不良反应退出治疗组,2例患者因不良反应退出对照组。与治疗前比较,两组治疗72周后24 h尿蛋白定量、ds-DNA抗体滴度、系统性红斑狼疮疾病活动指数(SLEDAI)评分均显著降低(P<0.05)。治疗组总缓解率为85.2%,对照组总缓解率为57.7%(P<0.05);DTE总有效率分别为59.3%和30.8%(P<0.05)。
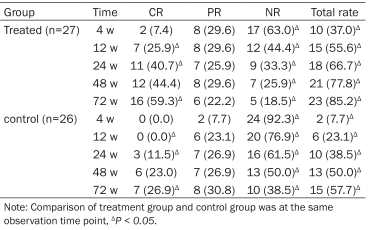
表1 治疗4、12、24、48和72周时两组总缓解率的比较[n(%)]
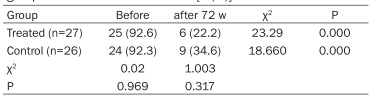
表2 治疗72周时两组ds-DNA阳性率的比较[n(%)]
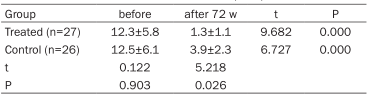
表3 两组治疗72周前后的SLEDAI评分比较(_x±s)
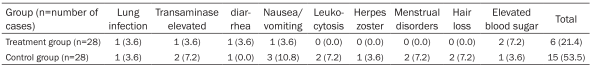
表4 两组的不良反应[n(%)]
结论:多靶点治疗III+V型或IV+V型狼疮性肾炎总缓解率高,治疗时间短,不良反应发生率低。
原文出处: Ye F, Wang S, Wang M, et al.Clinical analysis of multi-target treatment for complex lupus nephritis.Am J Transl Res 2022;14(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#多靶点#
41
#狼疮#
29
#肾炎#
36
#复杂性#
61
学习
57