AJKD:伴有房颤的CKD患者口服抗凝剂疗效分析
2021-04-18 MedSci原创 MedSci原创
在预防伴有AF和轻中度肾脏疾病患者血栓栓塞事件和出血风险方面DOACs优于华法林。值得注意的是,使用OAC可能会增加出血风险,对于伴有AF的透析患者并无明显益处。
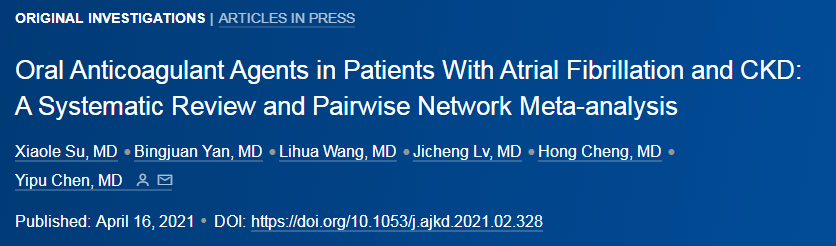
近日,肾脏病学权威杂志Am J Kidney Dis上发表了一篇研究文章,该研究旨在评估不同口服抗凝血剂(OAC)对伴有心房颤动(AF)和慢性肾病(CKD)患者的相对疗效和安全性。

研究人员进行了系统评价和成对以及贝叶斯网络元分析。参与者为伴有AF和3-5D期CKD成年患者,他们接受了OACs治疗。研究人员纳入了肾小球过滤速率(GFR)<60ml/min患者亚组疗效和安全结局的随机对照试验(RCT)和观察性研究。两位审稿人独立提取数据,评估了研究质量,并评定了证据强度(SOE)。研究人员使用受限制的最大似然方法的随机效果模型拟合贝叶斯框架内的成对Meta分析以及网络Meta分析。
成对荟萃分析纳入了8项RCT和46项观察性研究,其分析结果表明,在预防血栓栓塞事件方面直接作用的口服抗凝血剂(DOACs)优于华法林(HR为0.86; 95%CI为0.78-0.95),并且没有异质性(I2=10.5%);DOACs可降低伴有AF和GFR为15-60ml/min患者的出血事件(0.81; 0.66-0.99)风险,并具有较大的异质性(I2=69.8%)。
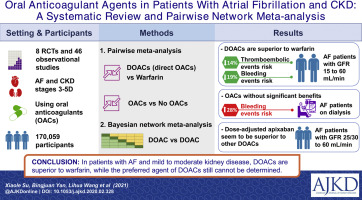
贝叶斯网络荟萃分析纳入了8项RCT,其分析结果表明剂量调整的阿哌沙班和15mg剂量的依度沙班在减少出血事件方面优于其它OAC治疗方案。剂量调整后的阿哌沙班比依度沙班在预防伴有AF和GFR为25/30-50ml/min患者出血性事件方面更有效。在伴有AF的透析患者中,与不使用抗凝血剂的患者相比,使用OAC治疗使出血风险增加了28%(1.28; 1.03-160)。
该研究的结果表明,在预防伴有AF和轻中度肾脏疾病患者血栓栓塞事件和出血风险方面DOACs优于华法林。值得注意的是,使用OAC可能会增加出血风险,对于伴有AF的透析患者并无明显益处。
原始出处:
Xiaole Su,et al.Oral Anticoagulant Agents in Patients With Atrial Fibrillation and CKD: A Systematic Review and Pairwise Network Meta-analysis.Am J Kidney Dis.2021.https://doi.org/10.1053/j.ajkd.2021.02.328
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#疗效分析#
37
学习了
53
学习了
49
有用
65
#CKD患者#
54
#口服抗凝剂#
25
了解...emmm
65
房颤,临床上碰到很多哦
33
谢谢梅斯提供这么好的信息,学到很多
46