Cell Death Dis:前列腺癌微环境中雄激素受体/丝胺A复合物的靶向作用
2021-02-12 AlexYang MedSci原创
前列腺癌是男性癌症相关死亡的主要原因,患者经常出现耐药性和转移性疾病。大多数研究集中在与雄激素受体突变有关或与前列腺癌细胞过度激活信号通路的获得特性有关的激素耐药机制。肿瘤微环境在前列腺癌的进展中起着
前列腺癌是男性癌症相关死亡的主要原因,患者经常出现耐药性和转移性疾病。大多数研究集中在与雄激素受体突变有关或与前列腺癌细胞过度激活信号通路的获得特性有关的激素耐药机制。肿瘤微环境在前列腺癌的进展中起着至关重要的作用。然而,涉及癌症相关成纤维细胞中雄激素/雄激素受体信号传导的机制以及对前列腺癌进展的后果仍然不清楚。
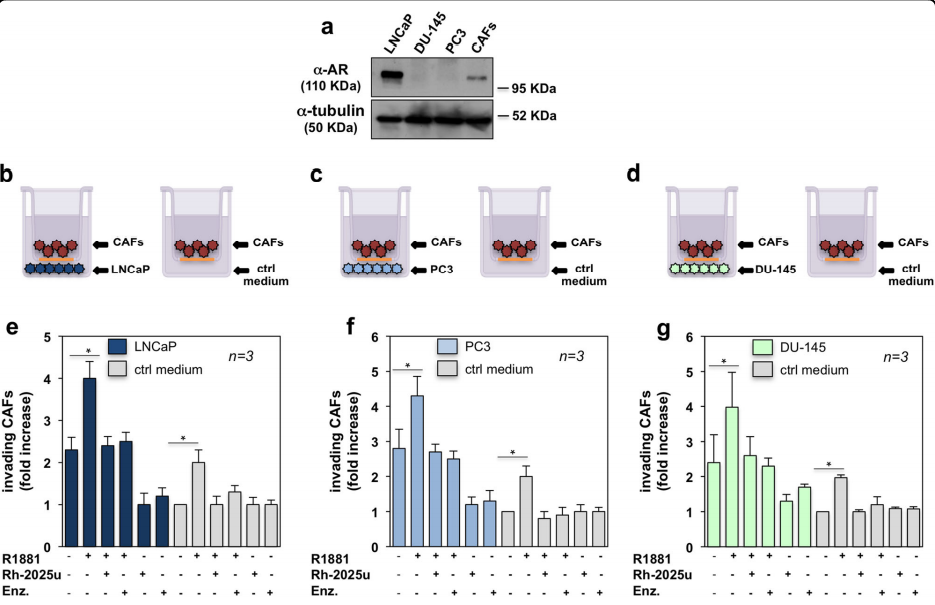
最近,有研究人员报道了前列腺癌相关成纤维细胞表达了一种转录无能的雄激素受体。当雄激素挑战时,该受体与支架蛋白filamin A在成纤维细胞的核外隔室共定位,从而介导其迁移和侵袭性。癌症相关的成纤维细胞在2D和3D培养物中向前列腺上皮癌细胞移动,从而诱导前列腺癌器官大小的增加。雄激素通过雄激素受体/丝胺A复合物在癌症相关成纤维细胞中的组装来增强这上述效应。一种雄激素受体衍生的钉状肽能够破坏雄激素受体/丝胺A复合物的组装,消除了癌症相关成纤维细胞的雄激素依赖性迁移和侵入性。值得注意的是,该肽在2D模型中削弱了雄激素诱导的CAFs的侵袭,并在雄激素处理的3D共培养中减少了整体肿瘤面积。雄激素受体与β1整合素和膜型-基质金属蛋白酶1联合激活蛋白酶级联,触发细胞外基质重塑。该肽还能损害雄激素对该级联的激活。
最后,研究人员指出,研究提供了一种潜在的新标志物--雄激素受体/丝胺A复合物,以及一种靶向前列腺癌相关成纤维细胞中雄激素/雄激素受体轴激活的细胞内通路的新治疗方法。该策略单独或与传统疗法联合使用,可能会使前列腺癌的治疗更加有效。
原始出处:
Marzia Di Donato , Alice Zamagni , Giovanni Galasso et al. The androgen receptor/filamin A complex as a target in prostate cancer microenvironment. Cell Death Dis. Jan 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Dis#
43
#靶向作用#
49
#CEL#
36
#复合物#
43
#Cell#
37
#雄激素受体#
32
#Death#
37
前列腺癌相关研究,学习了,谢谢梅斯
49