OCC 2020丨彭道泉:强化降脂在超高危ASCVD患者中聚焦斑块逆转价值和新趋势
2020-06-02 心关注 心关注
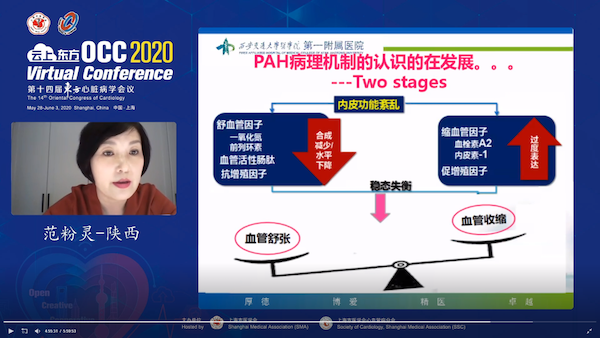
2020年5月29日,在第十四届东方心脏病学会议(OCC 2020)云上东方直播平台上,中南大学湘雅二医院彭道泉教授在血脂-动脉粥样硬化论坛 “从斑块逆转看强化降脂在超高危ASCVD患者中
众所周知,LDL颗粒在血管内皮下聚集是斑块形成的必备条件。巨噬细胞可通过各种机制识别和吞噬“凋亡细胞(AC)”,过多LDL沉积会诱发更多的AC,超过其巨噬细胞的吞噬能力,斑块会不断增长。而通过积极降脂治疗,斑块内的脂质减少,AC减少,AC清除大于AC 产生,斑块就会逆转。但不同时期的斑块巨噬细胞清除能力存在差异,晚期斑块胞葬能力受损,因此动脉粥样硬化越早干预逆转越快,越晚干预逆转越慢。
强效降低LDL-C至一定水平是实现斑块稳定逆转的必要条件
YELLOW研究证实,降脂越强化,斑块内脂质降低越多。强化降脂可显著减少血管壁的巨噬细胞,短时间内(如血脂洗脱治疗后3天)即可减轻血管壁的炎症反应,但要逆转斑块需要更长的时间。REVERSAL研究随访18个月发现,与中等强度他汀降脂治疗相比,高强度他汀降脂治疗显著抑制斑块进展。荟萃分析进一步明确,LDL-C水平降低与粥样斑块体积百分比(PAV)改变呈线性相关。ASTEROID研究显示,高强度他汀治疗使LDL-C从130 mg/dl降至LDL-C 水平60.8 mg/dl,使中位PAV降低0.79%,逆转斑块进展。SATURN研究结果证实,LDL-C降幅决定了斑块的逆转程度。对4项在美国、北美、欧洲、澳大利亚进行的随机试验数据合并进行的事后分析提示,强效降低LDL-C至一定水平是实现斑块稳定逆转的必要条件。
无论他汀还是非他汀类降脂药物治疗,LDL-C降至越低,斑块逆转越多
PRECISE-IVUS研究发现,他汀与非他汀类药物依折麦布联合强化降脂(LDL-C降至63.2 mg/dl)较他汀单药治疗显著逆转斑块进展。对降脂治疗试验进行荟萃分析证实,不论他汀还是非他汀类药物降脂治疗,LDL-C降至越低,斑块逆转越多;且PRECISE-IVUS研究联合治疗组中急性冠脉综合征(ACS)患者的斑块逆转最为显著,揭示风险更高的“脆弱”患者,LDL-C水平与粥样斑块改变的联系更密切。
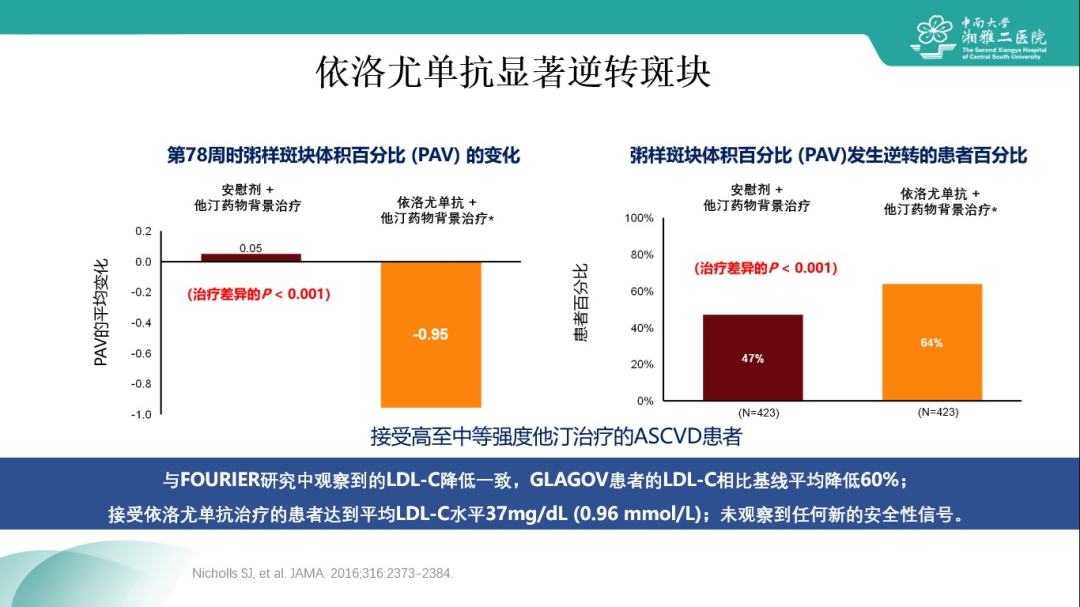
GLAGOV研究:依洛尤单抗使LDL-C进一步降至36.6 mg/dl,显著逆转斑块
新型降脂药物PCSK9抑制剂能够带来更强效的LDL-C降低,其在斑块逆转方面的表现如何?GLAGOV研究是一项多中心、双盲、随机对照临床试验,纳入968例有症状性的冠状动脉疾病(CAD)患者,冠脉造影显示靶血管20%~50%狭窄,采用IVUS评估斑块进展或消退情况。患者在他汀治疗基础上随机分配接受依洛尤单抗或安慰剂治疗,结果发现,治疗78周后,依洛尤单抗组平均LDL-C大幅降至36.6 mg/dl(vs.他汀单药组93.0 mg/dl,P<0.001),LDL-C绝对降低为56.3 mg/dl,较基线降幅为59.8%(图1);依洛尤单抗的主要终点即治疗78周后相对基线的斑块体积百分比(PAV)变化为降低0.95%(与基线相比,P<0.001;与安慰剂组比,P<0.001);且依洛尤单抗组相对安慰剂组有更多患者发生斑块逆转(64% vs. 47%,P<0.001)(图2)。GLAGOV研究中观察到的依洛尤单抗带来的LDL-C降低(相对基线平均降低60%)与FOURIER研究一致,且未观察到任何新的安全性信号,同样证实了依洛尤单抗强效降低LDL-C且安全性良好的特性。

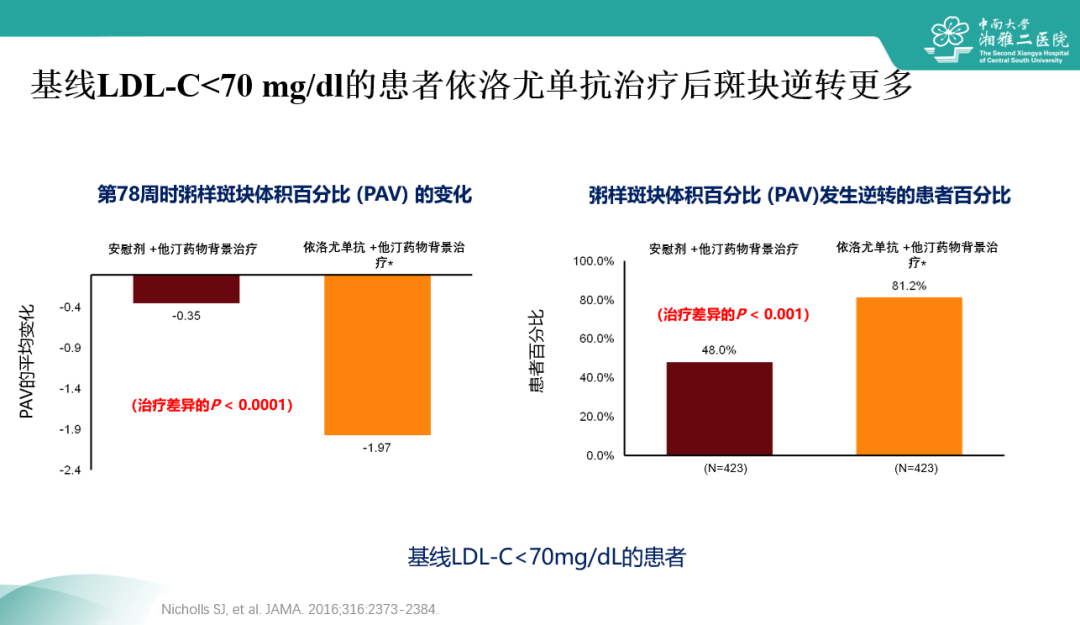
GLAGOV研究亚组:基线LDL-C<70 mg/dl的患者可从依洛尤单抗治疗中得到更大斑块逆转获益
GLAGOV研究中,对基线LDL-C低于70 mg/dl的患者,依洛尤单抗可使LDL-C进一步降低至24 mg/dl,且可实现更为显著的斑块逆转:PAV降低更明显(-1.97 vs. 安慰剂组-0.35,P<0.0001),且更大比例(81.2% vs. 48%,P<0.001)患者得以实现斑块逆转(图3)。
对所有接受连续IVUS评价的患者所达到的LDL-C水平和PAV变化间的关联(及95%CI)进行局部回归 (LOESS) 曲线分析显示,治疗所达到的LDL-C水平和PAV变化的关系无平台效应(图4),提示将LDL-C水平降得越低,PAV变化越大,斑块逆转越显著。

小结:超高危ASCVD患者及早联合PCSK9抑制剂,更快实现斑块稳定逆转,更早得到心血管获益
LDL-C是动脉粥硬化性心血管疾病(ASCVD)的关键致病因素,降低LDL-C可减少斑块内脂质和其诱导的炎症细胞凋亡,使凋亡细胞清除处于优势,利于斑块逆转。临床研究和荟萃分析结果提示,不论他汀类药物或非他汀类降脂药物,LDL-C下降越低,斑块逆转越多。PCSK9抑制剂依洛尤单抗一上市,便以大幅降低LDL-C水平的作用和良好的安全性备受关注,其稳定逆转斑块的作用在GLAGOV研究中得到明确证实,这种改善最终会转化为心血管事件减少的获益,而这种获益已经在里程碑式的FOURIER研究中得到明确证实。联合降脂尤其是联合PCSK9抑制剂会是未来强化降脂的一种重要手段和新趋势,对适宜患者尤其是超高危ASCVD患者,及早启用PCSK9抑制剂联合,将有助于更快实现斑块稳定逆转,更早得到心血管事件获益。
专家简介
彭道泉
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#ASC#
35
#ASCVD#
48
#斑块#
35
#OCC#
37
#OCC 2020#
42