AHA发布脑静脉血栓形成新指南
2011-02-21 MedSci原创 MedSci原创
美国心脏学会(AHA)和美国卒中学会(ASA)2011年2月3日发布了首个关于脑静脉血栓形成的科学声明。声明中的建议有助于临床医师发现这种主要见于年轻卒中患者的罕见病因。 “脑静脉血栓形成的诊断和处理需要一个高水平的怀疑”,委员会主席Gustavo·Saposnik博士说。“指南就是要提高对这类疾病的察觉与识别。” 委员会包括一个来自美国、加拿大、墨西哥、葡萄牙和阿根廷的多学科专家
美国心脏学会(AHA)和美国卒中学会(ASA)2011年2月3日发布了首个关于脑静脉血栓形成的科学声明。声明中的建议有助于临床医师发现这种主要见于年轻卒中患者的罕见病因。
“脑静脉血栓形成的诊断和处理需要一个高水平的怀疑”,委员会主席Gustavo·Saposnik博士说。“指南就是要提高对这类疾病的察觉与识别。”
委员会包括一个来自美国、加拿大、墨西哥、葡萄牙和阿根廷的多学科专家组。指南于2011年2月3日在线发表于《Stroke》杂志。指南得到了美国神经病学学会、美国神经外科医师学会、神经外科医师大会、伊比利亚-美洲卒中学会以及神经介入外科学会的认可。
脑静脉血栓形成由硬脑膜静脉窦血凝块引起,占所有卒中的0.5%-1%,多见于孕妇、服用口服避孕药的女性以及45岁及以下的年轻人群。
根据指南所述,在西方国家,妊娠期间和产后脑静脉血栓形成的发病率为1:2500—1:10000。
风险最大的时期是妊娠晚期和产后前4周。女性中,73%的脑静脉血栓形成发生在刚刚分娩后。但是,指南作者指出,脑静脉血栓形成并非再次妊娠的禁忌。
指南建议,一旦患者被怀疑有脑静脉血栓形成,应进行血液检查,以明确是否存在促血栓形成因素,如C蛋白或S蛋白、抗凝血酶缺乏、抗磷脂综合征、凝血酶原G20210A突变和凝血因子V Leiden。
大约30%到40%的脑静脉血栓形成患者可能发生颅内出血。“鉴别出血是由于脑动脉破裂引起还是由脑静脉血栓形成引起非常重要”,Saposnik博士说。“因为它们的出血发病机制和治疗方式完全不同。”指南建议,有脑出血但病因不明的患者应行脑静脉影像学检查。
根据脑静脉和硬脑膜窦血栓形成的国际研究,头痛是最常见的症状。根据记录,有90%的患者发生头痛。(Stroke. 2005;36:1720–1725).
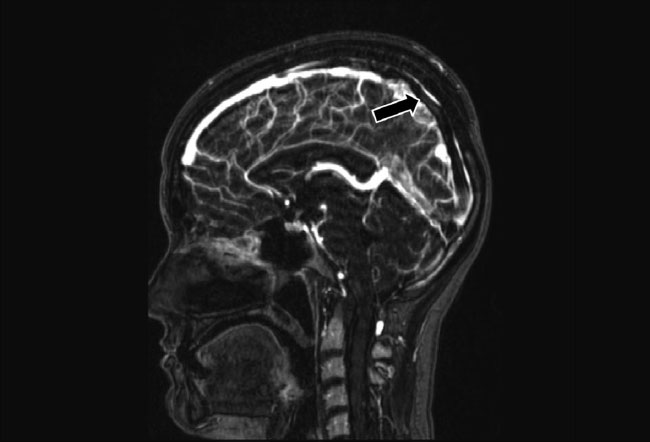
“常用的恰当的急性治疗包括预防并发症和抗凝治疗”,Saposnik博士说。指南强调,磁共振成像(MRI)和磁共振静脉造影是最敏感、因此也是推荐使用的检查方式。在急诊室,当无法实施MRI时,CT可能会有用。
Saposnik博士指出,关于脑静脉血栓形成患者血管内治疗或溶栓治疗的证据有限。基于此,当前指南建议,只有对采用了最佳内科治疗方法、但其神经功能仍渐进性恶化的患者,才使用该治疗。
“如同所有其他指南一样”,Saposnik博士说。“当前指南提供的是对现有证据分析所得的总体方法,并不针对个体化情况。”
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#新指南#
29
#静脉#
37
#静脉血#
39
#AHA#
34
#静脉血栓形成#
50