背景
在剖宫产术中,给予最佳剂量的麻醉剂以确保足够的麻醉深度,同时避免对胎儿产生不良影响是非常重要的。在一些国家,硫喷妥钠仍然是产科手术麻醉诱导的首选药物。我们的研究目的是比较两种不同剂量的硫喷妥纳对产妇麻醉深度和新生儿状况的影响。
方法
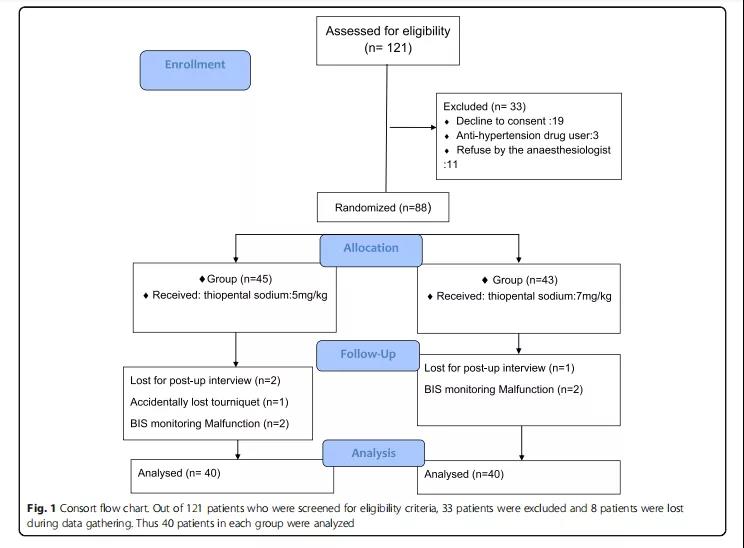
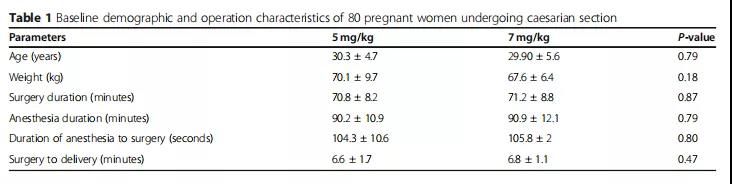
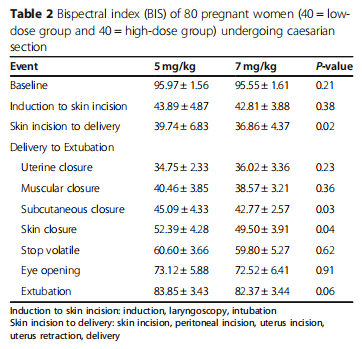
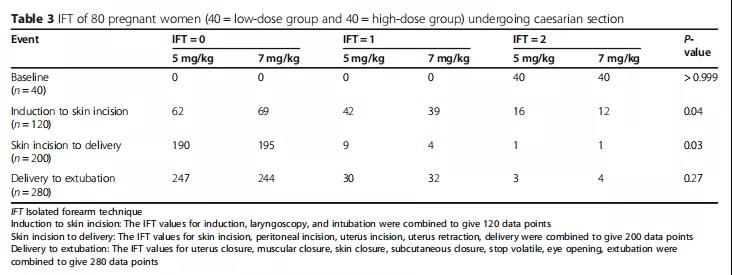
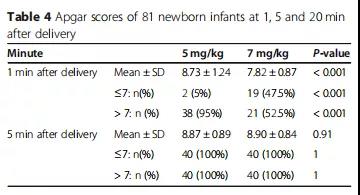
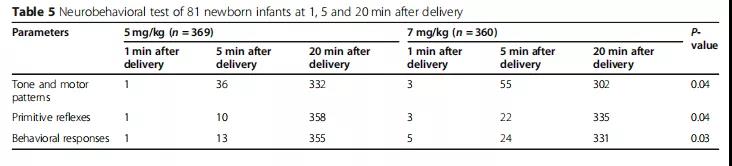
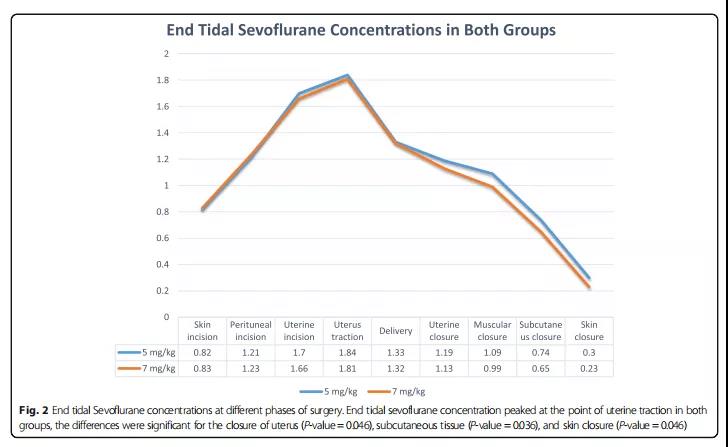
在这项临床试验中,我们把接受择期剖宫产术的产妇随机分为两组,分别接受低剂量(5mg/kg)和高剂量(7mg/kg)的硫喷妥钠。选用2mg/kg琥珀胆碱作肌肉松弛剂,用O2/N2O和七氟醚进行维持麻醉。在不同阶段,使用孤立前臂技术(IFT)和脑电双频指数(BIS)评估麻醉深度。此外,使用Apgar评分和神经行为测试对婴儿健康状况进行评估。
结果
每组有40名产妇接受评估,高剂量组在分娩前切开皮肤时、皮肤缝合时BIS显着降低。此外,在孤立前臂技术的使用中,两组产妇诱导后切皮时和分娩时作出的回应也存在显着差异。分娩1分钟后,高剂量组新生儿的Apgar评分明显降低。低剂量组新生儿在神经行为测试的三个领域结果都显着较好。
结论
7mg/kg的硫喷妥钠可以为母亲创造更深层次镇静的效果,作用优于5mg/kg浓度的硫喷妥钠。但是,它对新生儿的Apgar评分和神经行为测试结果有负面影响。作为剖宫产术中可使用的麻醉剂,硫喷妥钠似乎已经过时了。
原始出处:
Golnar Sabetian, Farid Zand, Fatemeh Mirhadi,et al. Adequacy of maternal anesthesia depth with two sodium thiopental doses in elective caesarean section: a randomized clinical trial.[J]. BMC Anesthesiology (2021) 21:201:1.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#EST#
36
临床研究
42
#随机临床试验#
43
#BMC#
42
#ESI#
40
高质量研究,读起来真爽,谢谢梅斯
62