BJU Int:接受膀胱切除术的肉瘤状分化患者的病理和肿瘤学结果
2021-05-12 AlexYang MedSci原创
最近,有研究人员在接受根治性膀胱切除术的患者中,与没有变异组织学的尿路上皮癌相比,具有肉瘤分化的尿路上皮癌是否与新辅助化疗较低的病理反应率和较差的肿瘤学结果有关。
最近,有研究人员在接受根治性膀胱切除术的患者中,与没有变异组织学的尿路上皮癌相比,具有肉瘤分化的尿路上皮癌是否与新辅助化疗较低的病理反应率和较差的肿瘤学结果有关。

研究人员鉴定了1995-2018年接受膀胱切除术的尿路上皮癌患者,并选择了经尿道切除术或膀胱切除术时有肉瘤分化的患者和没有组织学变异的患者。从≥cT2降至≤pT1N0定义为部分反应;降至pT0N0定义完全反应。
研究共包括了131名肉瘤分化的患者和1722名无变异组织学的患者,其中25名活检时有肉瘤组织学的患者和313名无变异组织学的患者接受了新辅助化疗。那些有肉瘤分化的患者呈现出更高的一致肿瘤分期(94%≥T2 vs 62%,P<0.001),因此更有可能接受新辅助化疗(29% vs 18%,P=0.004)。研究人员没有发现证据支持经尿道切除的肉瘤组织学患者和纯尿路上皮癌患者在部分反应(24% vs 31%)或完全反应(20% vs 24%)方面存在差异(P=0.6)。在肉瘤分化的患者中,接受NAC的患者五年无复发生存率为55%(95%CI为41%-74%),单独接受膀胱切除的患者为40%(95%CI为31%-52%)(P=0.1)。调整了分期、结节受累、边缘状态和接受新辅助化疗后,肉瘤分化与更差的无复发(HR 1.83,95%CI 1.39-2.40)、疾病特异性(HR 1.66,95%CI 1.24-2.23)和总生存(HR 1.38,95%CI 1.06-1.78)有关。
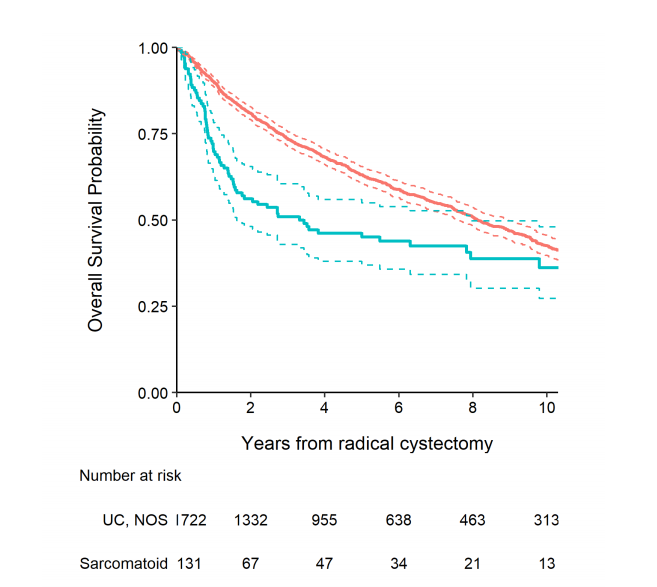
根治性膀胱切除术后的总生存
最后,研究人员指出,肉瘤分化与发病时的较高阶段有关,并与较差的生存期独立相关。如果在初次切除时发现肉瘤分化,则有类似的病理反应率,而且接受NAC的患者生存率更高,因此似乎有必要使用NAC治疗。另外,研究人员指出需要对这种组织学的不良结果的其他驱使因素进行调查。
原始出处:
Nima Almassi, Emily A Vertosick, Daniel D Sjoberg et al. Pathologic and oncologic outcomes in patients with sarcomatoid differentiation undergoing cystectomy. BJU Int. Apr 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#切除术#
40
👍
64
#肿瘤学#
37
#膀胱切除术#
46
学习
62
好文章!
55
受益匪浅
57