NEJM:CYP2C19功能缺失携带者服用替格瑞洛与氯吡格雷对卒中或TIA的比较分析
2021-12-30 MedSci原创 MedSci原创
在携带CYP2C19功能缺失等位基因的轻度缺血性卒中或TIA的中国患者中,替格瑞洛治疗后90天卒中风险略低于氯吡格雷。两个治疗组的重度或中度出血风险没有差异,但替格瑞洛与氯吡格雷相比,总出血事件更多。
目前,尚未广泛开展针对替格瑞洛和氯吡格雷对CYP2C19功能缺失携带者进行卒中二级预防效果的比较。

近日,顶级医学期刊NEJM上发表了一篇研究文章,研究人员在中国202个中心进行了一项随机、双盲、安慰剂对照试验,纳入了携带CYP2C19功能缺失等位基因的轻度缺血性卒中或短暂性脑缺血发作(TIA)患者。
患者在症状出现后24小时内以1:1的比例分配接受替格瑞洛(第1天180mg,然后在第2天至第90天每天两次,每次剂量为90mg)和安慰剂氯吡格雷治疗,或接受氯吡格雷(第1天300mg,然后在第2天至第90天每天服用75mg)和安慰剂替格瑞洛治疗;两组均服用阿司匹林治疗21天。该研究的主要疗效结局是新发卒中,主要安全性结局是90天内重度或中度出血。
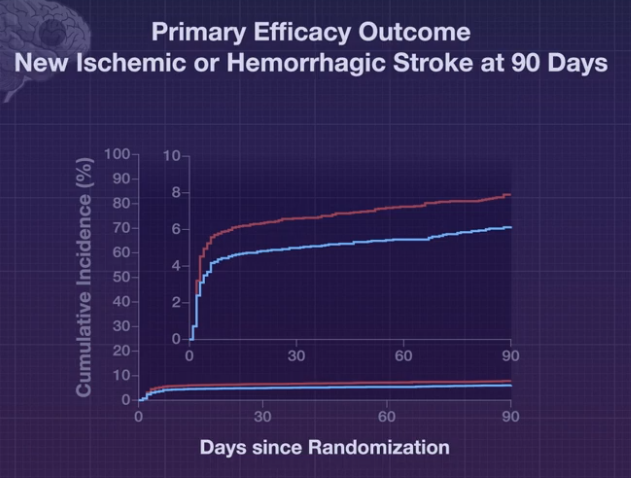
该研究总共筛选了11255名患者,共纳入了6412名患者,其中替格瑞洛组3205名患者,氯吡格雷组3207名患者。患者的中位年龄为64.8岁,33.8%为女性;98.0%属于汉族。替格瑞洛组191名患者(6.0%)和氯吡格雷组243名患者(7.6%)在90天内发生卒中(风险比为0.77;95%置信区间为0.64至0.94;P=0.008)。次要结局通常与主要结局方向相同。替格瑞洛组9例患者(0.3%)和氯吡格雷组11例患者(0.3%)发生重度或中度出血;分别有170名(5.3%)患者和80名(2.5%)患者出现任何出血。
由此可见,在携带CYP2C19功能缺失等位基因的轻度缺血性卒中或TIA的中国患者中,替格瑞洛治疗后90天卒中风险略低于氯吡格雷。两个治疗组的重度或中度出血风险没有差异,但替格瑞洛与氯吡格雷相比,总出血事件更多。
原始出处:
Yongjun Wang,et al.Ticagrelor versus Clopidogrel in CYP2C19 Loss-of-Function Carriers with Stroke or TIA.NEJM.2021.https://www.nejm.org/doi/full/10.1056/NEJMoa2111749
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#携带者#
46
#氯吡格雷#与#替格瑞洛#
69
#比较分析#
40
#CYP2C19#
37
非常感谢
62