皮瓣移植围手术期是否应该停止双联抗血小板治疗?
2022-01-11 MedSci原创 MedSci原创
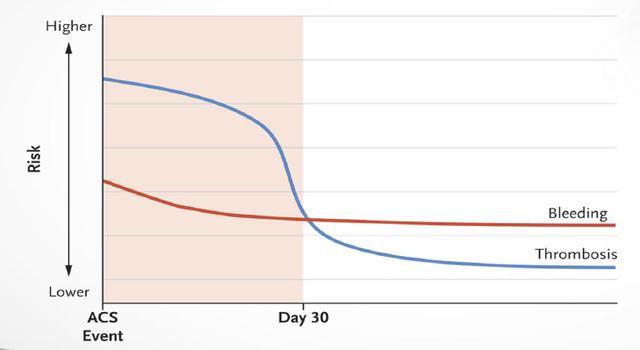
由于担心出血,围手术期通常不使用抗血小板药物。双重抗血小板治疗,如阿司匹林和氯吡格雷,对缺血性心脏病或外周血管疾病患者有明显的发病率和死亡率优势。
由于担心出血,围手术期通常不使用抗血小板药物。双重抗血小板治疗,如阿司匹林和氯吡格雷,对缺血性心脏病或外周血管疾病患者有明显的发病率和死亡率优势。
本研究旨在评估围手术期双重抗血小板治疗对下肢自由组织转移人群的影响。该研究对资深作(K.K.E.)2011年至2019年进行的下肢游离组织移植进行回顾性研究。
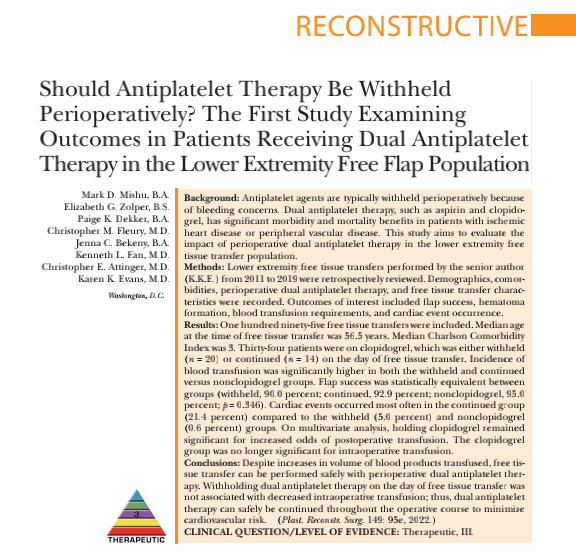
图1 文章来源
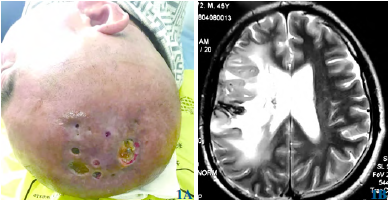
记录了人口统计学、合并症、围手术期双重抗血小板治疗和自由组织转移的特点。所关注的结果包括皮瓣成功、血肿形成、输血需求和心脏事件的发生。
结果共统计了195例游离皮瓣移植。在进行游离皮瓣移植时,年龄中位数为56.5岁。中位数的Charlson并发症指数为3。
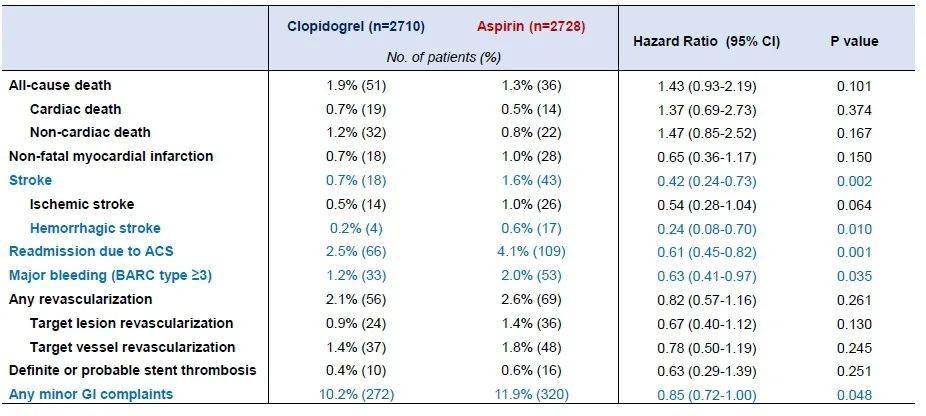
34名患者正在服用氯吡格雷,但在游离皮瓣移植的当天有20名没有服用,或14名继续服用。输血的发生率在暂停使用和继续使用中都显著升高,而与非氯吡格雷组相比,输血的发生率都显著较高。
在统计学上,各组的皮瓣成功率相当,组之间在统计学上是相等的(暂停使用,90.0%;继续使用,92.9%;非氯吡格雷,95.0 百分比;P = 0.346)。
心脏事件在继续治疗组中最常发生 (21.4%),而暂停治疗组(5.0%)和非氯吡格雷组(0.6 (0.6%)组较少。
在多变量分析中,服用氯吡格雷仍然有可能增加术后输血的几率,但但对术中输血影响不大。

尽管输血量增加,但在围手术期双抗血小板治疗的情况下,可以安全地进行自由组织转移。在游离皮瓣移植的当天停止双联抗血小板治疗与术中输血量减少无关。
因此,双联抗血小板治疗可以在整个手术过程中安全地继续进行。疗法可以在整个手术过程中安全地继续下去,以尽量减少心血管风险。
原始文章:
Mishu Mark D,Zolper Elizabeth G,Dekker Paige K et al. Should Antiplatelet Therapy Be Withheld Perioperatively? The First Study Examining Outcomes in Patients Receiving Dual Antiplatelet Therapy in the Lower Extremity Free Flap Population.[J] .Plast Reconstr Surg, 2022, 149: 95e-103e.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#手术期#
0
#皮瓣移植#
41
#双联抗血小板#
44
赞
43
#皮瓣#
45
#双联抗血小板治疗#
33