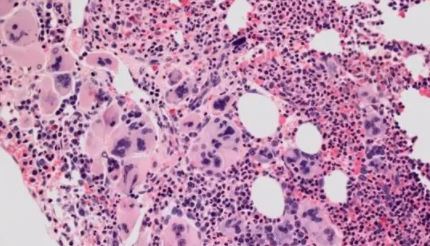
JAMA Oncol:Elotuzumab联合每周KRd治疗新诊断的多发性骨髓瘤
2022-08-03 MedSci原创 MedSci原创
在不进行ASCT的情况下,予以Elotuzumab和每周KRd联合治疗显示出了高sCR率和/或MRD阴性率,而且缓解持久。
与三联方案相比,采用由单克隆抗体、蛋白酶体抑制剂、免疫调节酰亚胺和皮质类固醇组成的四联方案治疗新诊断的多发性骨髓瘤 (NDMM) 可延长患者的无进展生存期。但是,最佳的四联方案,以及其是否能消除对一线自体干细胞移植(ASCT)的需要,仍未知。
该研究旨在评估埃罗妥珠单抗(Elotuzumab)和周用卡非佐米、来那度胺和地塞米松(Elo-KRd)治疗NDMM的疗效,无论是否可进行ASCT。
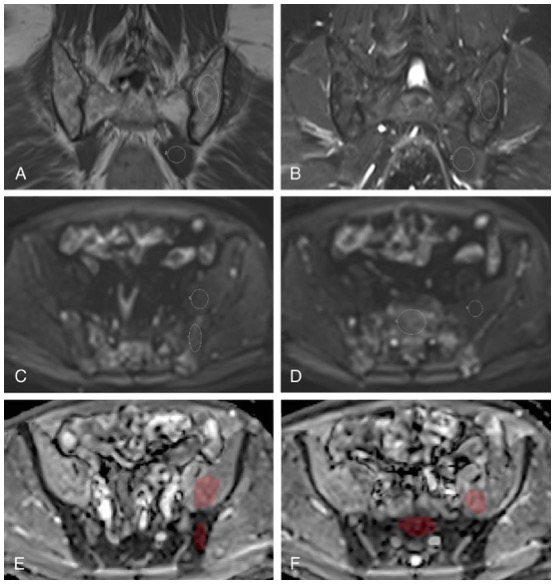
这是一项多中心、单臂的2期研究,予以受试患者12-24个疗程的Elo-KRd治疗;第8个疗程(C8)和第12个疗程后采用二代测序(NGS)检测MRD阴性与否以明确Elo-KRd的治疗疗程。主要终点是8个Elo-KRd疗程后的严格完全缓解率(sCR)和/或MRD阴性率(10-5)。次要终点包括安全性、缓解率、MRD状态、PFS和总生存率(OS)。
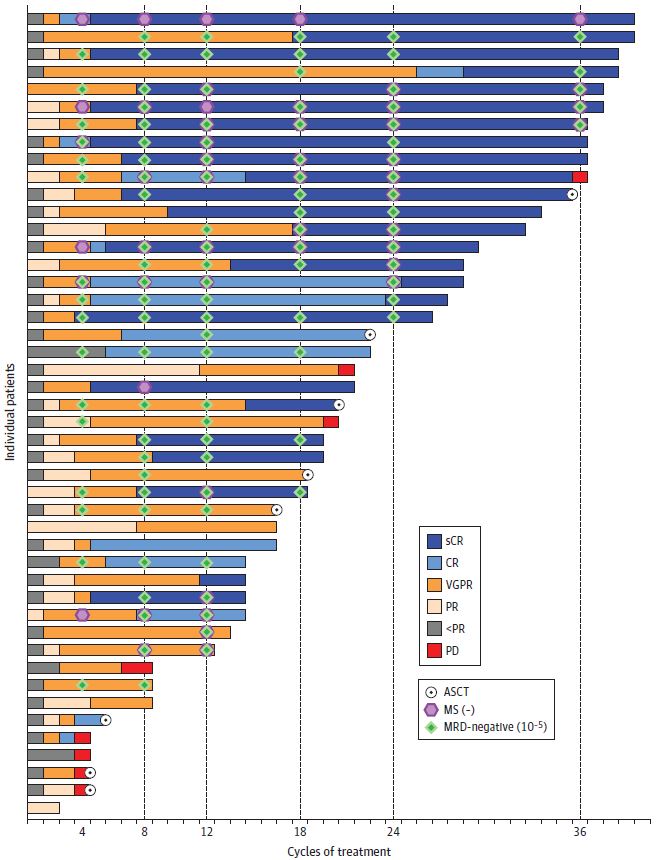
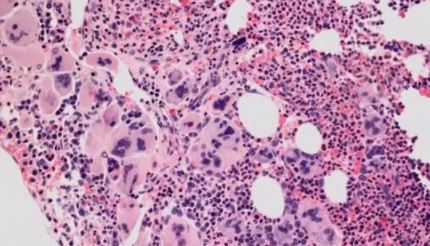
每位患者的缓解深度和持续时间
2017年7月-2021年2月期间,共招募了46位患者(中位年龄62岁,24%的患者>70岁)。总体上,32位患者(70%)是白种人,6位(13%)是黑人。33位(72%)男性,13位(28%)是女性。22位 (48%) 患者存在高危细胞遗传学异常。
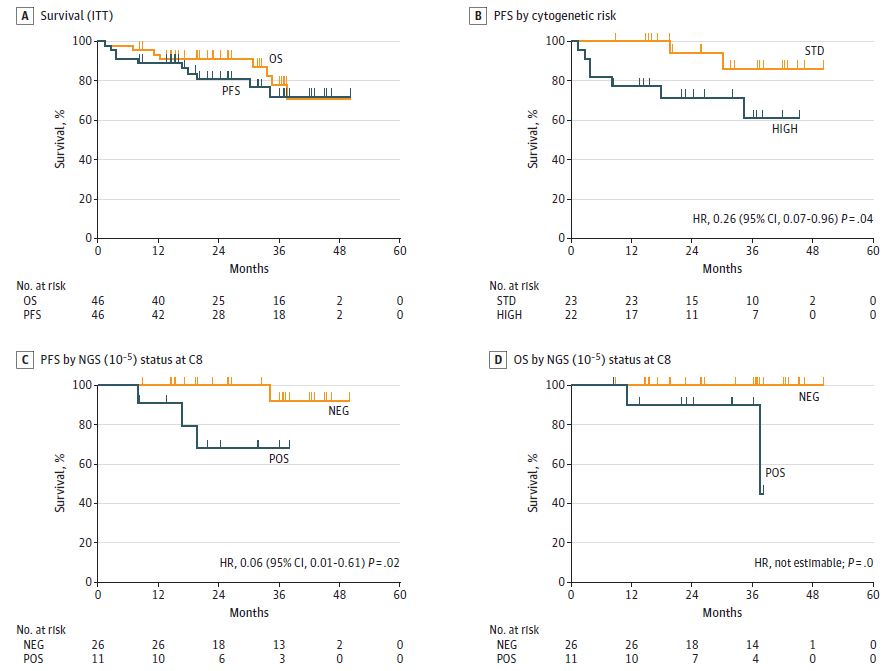
不同分组患者的生存预后
C8后,45位患者中有26位(58%)获得了sCR和/或MRD阴性,符合预设的统计学意义阈值。随着时间的推移,缓解不断加深,MRD阴性率增加到了70%,MS阴性率增加到了65%。
最常见(>10%)的3/4级不良反应有肺和非肺部感染(13%和11%)。此外,发生了一例5级心肌梗塞。预估的3年总PFS率是72%;C8后MRD阴性患者的预估3年PFS率是92%。
综上,在不进行ASCT的情况下,予以Elotuzumab和每周KRd联合治疗显示出了高sCR率和/或MRD阴性率,而且缓解持久。
原始出处:
Derman BA, Kansagra A, Zonder J, et al. Elotuzumab and Weekly Carfilzomib, Lenalidomide, and Dexamethasone in Patients With Newly Diagnosed Multiple Myeloma Without Transplant Intent: A Phase 2 Measurable Residual Disease-Adapted Study. JAMA Oncol. Published online July 21, 2022. doi:10.1001/jamaoncol.2022.2424
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#新诊断#
61
#Oncol#
61
#多发性#
36
#mAb#
32
#elotuzumab#
33
JAMA上文章都是顶级的,谢谢梅斯及时上新
0