JCO:阿美替尼对比吉非替尼对EGFR突变NSCLC一线治疗结果公布(AENEAS研究)
2022-05-19 豪森药业集团 豪森药业集团
2022年5月18日,国际著名肿瘤学期刊《临床肿瘤学杂志》(Journal of Clinical Oncology,JCO,IF:44.544)在线发表了上海交通大学附属胸科医院陆舜教授主导的翰森制
2022年5月18日,国际著名肿瘤学期刊《临床肿瘤学杂志》(Journal of Clinical Oncology,JCO,IF:44.544)在线发表了上海交通大学附属胸科医院陆舜教授主导的翰森制药创新药阿美乐®(甲磺酸阿美替尼片)AENEAS研究论文。这是ASCO官方期刊首次发表中国原创三代EGFR-TKI临床数据。 AENEAS是阿美替尼对比吉非替尼一线治疗EGFR敏感突变局部晚期或转移性NSCLC的随机、对照、Ⅲ期研究。该研究结果显示出阿美替尼用于一线治疗EGFR敏感突变阳性局部晚期或转移性NSCLC在安全性和有效性方面的卓越优势。 阿美乐®是翰森制药自主研发的首个中国原创三代EGFR-TKI。上市两年来,在临床上被广泛使用,累计惠及NSCLC患者十余万人,其卓越疗效和安全性赢得医生和患者一致赞誉。翰森制药集团执行董事吕爱锋表示:“阿美乐®Ⅲ期临床研究数据在JCO发表,体现了国际肿瘤学术界对阿美乐®的高度认可,这是中国医药创新在肺癌靶向治疗领域的重大突破。作为中国领先的创新驱动型制药企业,翰森制药将继续加快科技创新步伐,通过技术创新让民族医药为中国乃至全球患者带来更多获益。” 关于AENEAS研究 该研究是一项多中心随机双盲对照的Ⅲ期研究,关于阿美替尼对比吉非替尼作为一线针对EGFR敏感突变阳性局部晚期或转移性非小细胞肺癌患者的治疗,总计超过400例受试者参加。此项研究入组患者全部为中国患者,是首个三代 EGFR-TKI 药物针对中国肺癌患者一线治疗的随机对照研究,证据等级更高,更能反映中国肺癌患者的疾病状况。 关于阿美乐®(甲磺酸阿美替尼片) 阿美乐®(甲磺酸阿美替尼片)是由翰森制药自主研发的首个中国原创三代EGFR-TKI创新药,也是全球首个中位无进展生存期(mPFS)超过1年(二线使用)的三代 EGFR-TKI。其在既往经EGFR-TKI治疗时或治疗后出现疾病进展的,存在EGFR T790M突变阳性的局部晚期或转移性NSCLC成人患者治疗方面疗效显著。2020年3月,阿美乐®首个适应症获批上市,填补了中国三代 EGFR-TKI 空白;2021年12月,阿美乐®用于具有表皮生长因子受体(EGFR)外显子19缺失或外显子21(L858R)置换突变阳性的局部晚期或转移性非小细胞肺癌(NSCLC)成人患者一线治疗适应症获批,开启了中国原创三代EGFR-TKI一线治疗全新时代。
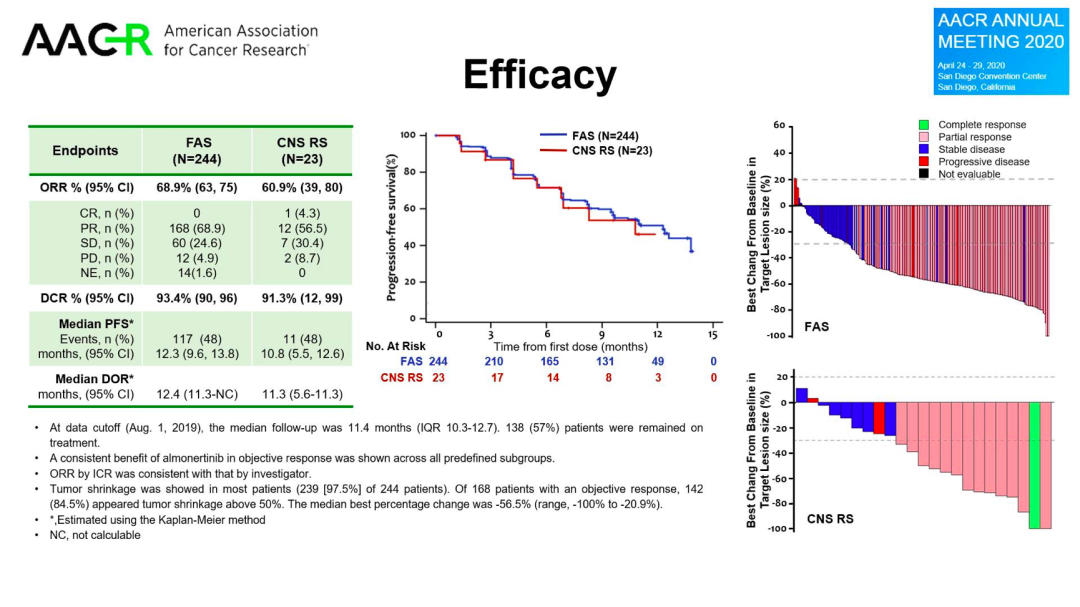
与现有的一线标准治疗药物吉非替尼相比,使用阿美替尼一线治疗的患者,无进展生存期(PFS)显著延长(中位PFS 19.3个月 VS 9.9个月),持续缓解时间(DoR)也显著延长(中位DoR 18.1个月 VS 8.3个月),阿美替尼显示出卓越的疗效。
在所有亚组人群中,阿美替尼中位PFS获益均优于吉非替尼:19del亚组20.8个月 VS 12.3个月(HR 0.39, P<0.0001), L858R亚组13.4个月 VS 8.3个月(HR 0.60, P=0.0102); 脑转移亚组的PFS获益尤为突出,为15.3个月 VS 8.2个月(HR 0.38, P<0.0001), 即可降低62%的疾病进展或死亡风险,相较之下无脑转移亚组为19.3个月 VS 12.6个月(HR 0.51, P<0.0001), 提示阿美替尼治疗可为脑转移患者带来更大获益。
在安全性方面,与吉非替尼组相比,阿美替尼组治疗持续时间更长(中位暴露时间463.5天 VS 254.0天), 但皮疹、腹泻、AST/ALT升高及治疗相关严重不良事件的发生率更低,提示阿美替尼一线治疗具有安全性优势。
作为首个全部入组中国患者的三代EGFR-TKI随机对照研究,AENEAS研究更能真实地反映中国患者的临床实际情况。2021年12月,该适应症已获国家药品监督管理局批准,成为阿美乐®第二个适应症。此前,AENEAS研究于2021年ASCO年会首次公布研究进展,获得国际同行广泛关注。2022年ASCO年会将进一步发布其脑转移亚组数据的最新进展。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#JCO#
50
#结果公布#
40
#GFR#
43
#治疗结果#
48
#阿美替尼##NSCLC#
122
#学习##心血管#
54
不错的文章
38