Emerg Microbes Infect:地塞米松治疗重症和危重型COVID-19患者的预后
2021-12-07 从医路漫漫 MedSci原创
自从SARS-CoV-2大流行的最初几个月以来,严重的新冠肺炎与全身炎症相关,这一事实促使人们努力评估抗炎和免疫调节的效果。新冠肺炎中激素的广泛抗炎作用已在众多试验中得到评估。
背景:自从SARS-CoV-2大流行的最初几个月以来,严重的新冠肺炎与全身炎症相关,这一事实促使人们努力评估抗炎和免疫调节的效果。新冠肺炎中激素的广泛抗炎作用已在众多试验中得到评估。幸运的是,康复试验显示地塞米松降低了新冠肺炎低氧血症患者的死亡率。地塞米松也与危重患者早日脱离呼吸机有关。包括RECOVER和其他6个临床试验在内的荟萃分析得出结论,全身应用皮质类固醇激素与较低的死亡率相关。最新指南建议新冠肺炎低氧血症患者使用地塞米松。地塞米松作为护理标准的实施代表着新冠肺炎快速发展的治疗战略中的一个里程碑。皮质类固醇治疗(CS-T)是唯一被证实可以降低新冠肺炎相关死亡率的干预措施,但在所有试验中,这样的结果并不一致。同样,关于继发感染的数据没有得到一致的评估,而且仍然缺乏。随着病例数量的持续增加,新冠肺炎仍然是全球卫生领域的一个主要问题。截至2021年10月31日,世界卫生组织报告的新冠肺炎确诊病例超过2.46亿例,死亡近500万例。我们进行了一项队列研究,以评估重症新冠肺炎患者实施CS-T前后的住院死亡率。
方法:我们在墨西哥城的一个新冠肺炎参考中心进行了一项前瞻性队列研究。我们中心使用电子病历对3月18日至11月9日期间连续入院的所有SARS-CoV-2实时聚合酶链反应(RT-PCR)阳性患者的数据进行前瞻性登记。包括重症和危重新冠肺炎的患者。根据以前的定义,当SpO2<93%,PaO2/FiO2<300时,呼吸频率≥为每分钟30次,或胸部CT显示≥50%受累时,被认为是重型;当休克、有创机械通气或多器官衰竭出现时,病例被认为是危重型。根据机构的规定,所有患者都接受了鼻咽拭子的SARS-CoV-2 RT-PCR检测。核酸提取使用NucliSens easyMAG系统(BioMérieux,Boxtel,荷兰)进行,RT-PCR在应用生物系统7500热循环仪(美国加利福尼亚州福斯特城)上根据其他地方描述的规范进行。对每个患者进行了从入院到死亡或出院的随访。主要结果是住院死亡。次要结果包括LOS、随访期间的IMV、IMV开始时间、IMV天数和培养证实的医院获得性感染(HAI)。传染病(ID)专家审查后考虑进行HAI,以确保其符合公认的标准。那些在出院或死亡前被转移到其他机构、LOS<24小时或被诊断为中度疾病的患者被排除在外。同时进行双变量、多变量和倾向分数匹配分析。
结果:1540例患者中,688例(45%)接受了冠状动脉造影,冠状动脉造影组的死亡率较低(18%对31%,p<0.01)。在IMV的患者中,CS-T组的死亡频率也较低(25%对55%,p<0.01)。CS-T组中位IMV时间较长(5天vs 3天,p<0.01)。糖化血红蛋白在糖化血红蛋白组发生率更高(20%对10%,p<0.01)。各组的LOS、IMV和IMV持续时间相似。多变量分析显示CS-T与较低死亡率之间存在独立联系(aOR 0.26,95%CI 0.19-0.36,p<0.001)。倾向评分匹配分析显示,CS-T与较低死亡率独立相关(aOR 0.33,95%可信区间0.22-0.50,p<0.01)。
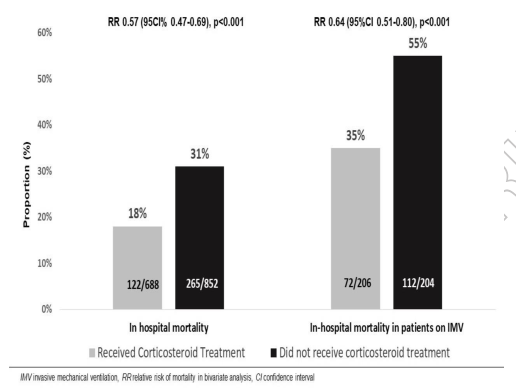
图1 住院死亡率
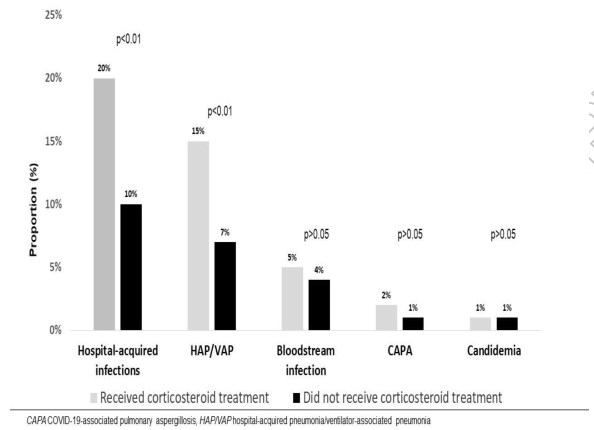
图2 医院获得性感染
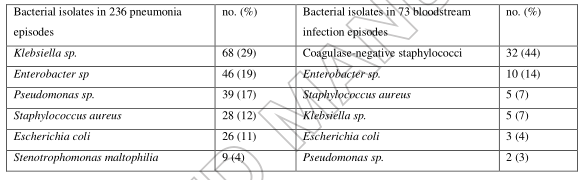
表 在整个队列的感染事件中分离到的细菌微生物。
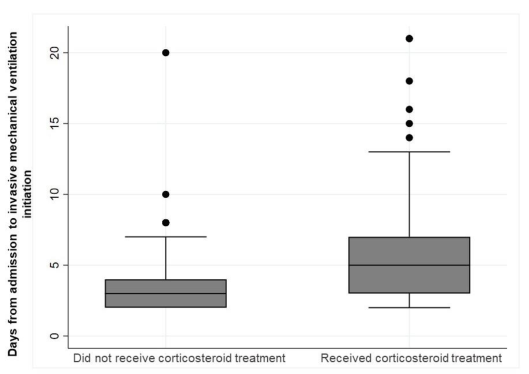
图3 入院至有创机械通气时间
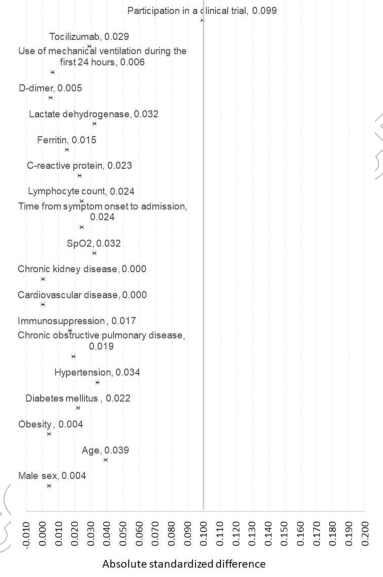
图4 配对指标的绝对标准差
结论:皮质类固醇治疗与重型和危重型新冠肺炎患者(包括IMV患者)的住院死亡率降低相关。
原文出处:
Martinez-Guerra BA, Gonzalez-Lara MF,et al.Outcomes of Patients with Severe and Critical COVID-19 Treated with Dexamethasone: a Prospective Cohort Study.Emerg Microbes Infect 2021 Nov 29
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CRO#
31
#Micro#
37
学习
53
学习
42
#COVID-19患者#
31
学习学习
58