J Gastroenterology H: 质子泵抑制剂的使用会导致脂肪肝的风险的增加
2021-05-30 MedSci原创 MedSci原创
抑制胃酸分泌的质子泵抑制剂-PPI是目前使用最为广泛的药物之一。虽然目前对于PPI的使用的临床反馈比较好,没有很强的副作用现象出现,但是已经有研究显示长期使用PPI会导致肠道菌群失调。
抑制胃酸分泌的质子泵抑制剂-PPI是目前使用最为广泛的药物之一。虽然目前对于PPI的使用的临床反馈比较好,没有很强的副作用现象出现,但是已经有研究显示长期使用PPI会导致肠道菌群失调,以及由此导致的一系列并发症的出现。脂肪肝,也称为肝脂肪变性,是一种常见的疾病,这是一种脂肪堆积过多的病症。随着肥胖症的流行,非酒精性脂肪肝(NAFLD)的全球患病率继续增加。酒精性肝病也是导致肝硬化、肝癌和肝功能衰竭的原因,本项研究旨在调查 PPI 使用与脂肪肝风险之间的关联。
研究人员收集了2002年1月1日至2015年12月31日间韩国国民健康保险服务国家样本库中的回顾性队列数据,该数据队列是一个基于全国人群的代表性样本。PPI 的使用情况是根据患者的处方药物中进行收集的,同时研究人员也对患者的脂肪肝变性进行了收集。

最后在1463 556人年的随访中,75727名患者至少使用了一种 PPI 处方药物,3735 名患者发生了脂肪肝并发症。研究结果显示PPI 使用者与非 PPI 使用者的脂肪肝病风险比为 1.68(95% CI,1.61–1.75)。当针对多个混杂因素(包括年龄、性别、体重指数、吸烟、饮酒、运动、收入水平和合并症)进行调整后,相关性仍然显着(HR,1.50;95% CI,1.44-1.57),使用 PPI 与脂肪肝风险增加相关。
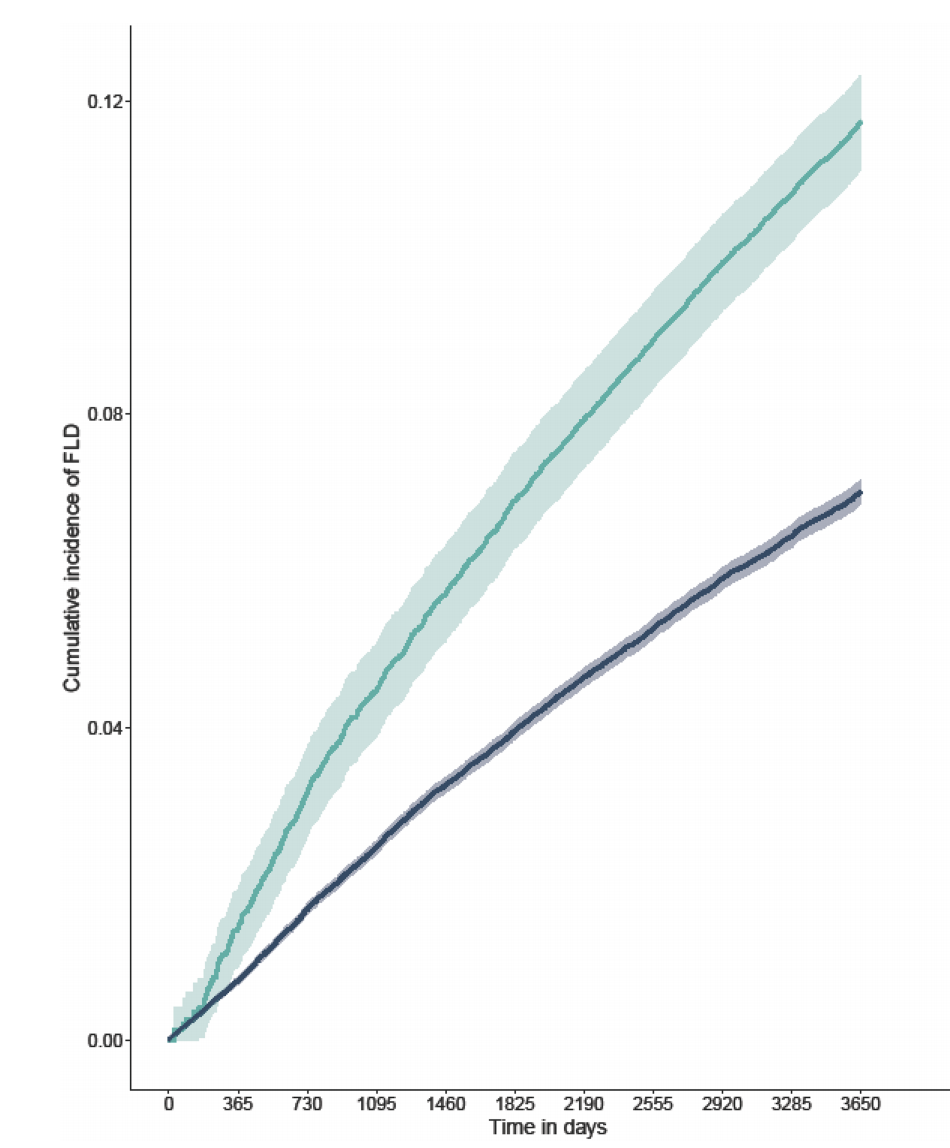
图:使用PPI后脂肪肝病发生风险
本项研究证实与不使用 PPI 的患者相比,使用 PPI 的患者与脂肪肝疾病风险增加有关。临床医生在开具 PPI 处方时应将脂肪肝视为PPI使用的潜在风险。
原始出处:
Jeung Hui Pyo. Et al. Proton pump inhibitors use and the risk of fatty liver disease: A nationwide cohort study. Journal of Gastroenterology and Hepatology. 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#AST#
37
#抑制剂#
29
#GAS#
27
#质子泵#
46
#Gastroenterol#
40
#Gastroenterology#
24