Cardiovasc Diabetol:血浆磷酸盐水平越高,糖尿病患者的死亡风险越高!
2022-05-09 Nebula MedSci原创
高血浆磷酸盐水平与 2 型糖尿病患者的全因死亡率升高相关
众所周知,2型糖尿病患者的心血管疾病风险显著升高。较高的血浆磷酸盐水平会促进血管钙化,这可能会对 2 型糖尿病患者的预后产生不利影响。研究人员推测,与非糖尿病患者相比,2 型糖尿病患者的血浆磷酸盐与其全因死亡率之间的相关性可能更强。
Van der Vaart等研究人员采用针对潜在混杂因素进行调整的多变量 Cox 回归分析了基于荷兰人群的 Lifelines 队列以及患有和不患有 2 型糖尿病的亚组中血浆磷酸盐与全因死亡率之间的相关性。
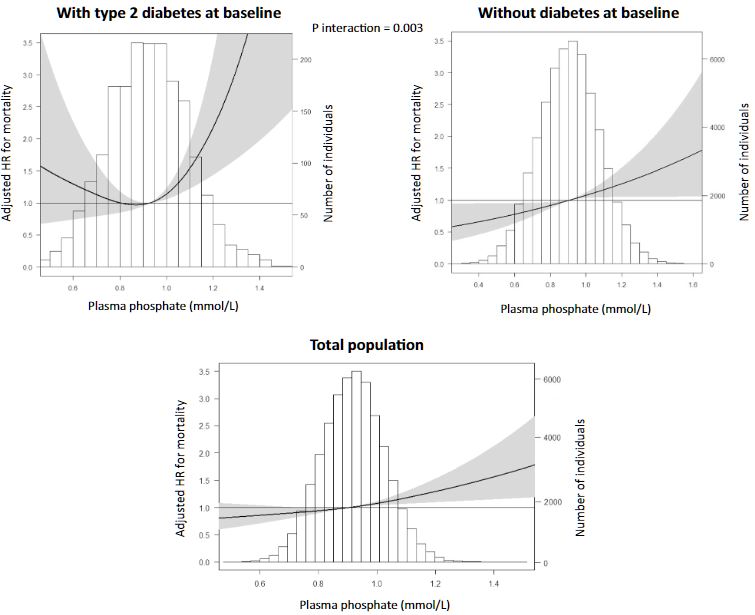
磷酸盐水平与不同人群全因死亡风险的相关性
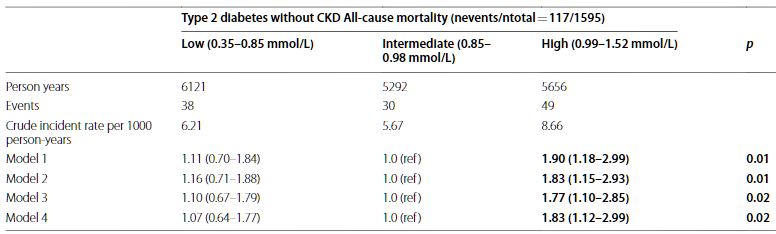
共纳入了57170位受试者,中位随访了9.4年。与磷酸盐最低三分位(0.85-0.99 mmol/L)组相比,最高三分位(1.00-1.83 mmol/L)组受试者的全因死亡风险更高(校正风险比[HR] 1.18,p=0.02)。基线 2 型糖尿病状态可显著改变上述相关性(p=0.003)。在 2 型糖尿病患者亚组(n=1790)中,磷酸盐最高三分位组受试者的全因死亡风险明显升高(与中间三分位组相比,HR 1.73,p=0.02)。在基线无糖尿病的亚组(n=55380)中,磷酸盐水平与死亡率无相关性(HR 1.12,p=0.14)。排除了估算的肾小球滤过率低于 60 mL/min·1.73 m2 的个体后,结果保持一致。
排除了eGFR<60 mL/min·1.73 m2 的个体后的分析结果
综上所述,高血浆磷酸盐水平与 2 型糖尿病患者的全因死亡率升高相关。在没有糖尿病的个体中,这种相关性较弱且无显著性。因此,应将血浆磷酸盐水平纳入 2 型糖尿病患者的健康监测项目;此外,降低磷酸盐水平是否可改善糖尿病患者的健康预后值得进一步研究。
原始出处:
van der Vaart, A., Cai, Q., Nolte, I.M. et al. Plasma phosphate and all-cause mortality in individuals with and without type 2 diabetes: the Dutch population-based lifelines cohort study. Cardiovasc Diabetol 21, 61 (2022). https://doi.org/10.1186/s12933-022-01499-4
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#BET#
44
#DIA#
45
#ASC#
48
#死亡风险#
45
#磷酸盐#
45
#糖尿病患者#
35