Neurology:中国原创研究-帕金森的运动表型和大脑皮层褶皱化息息相关
2021-04-04 Freeman MedSci原创
帕金森的运动表型和大脑皮层褶皱化息息相关

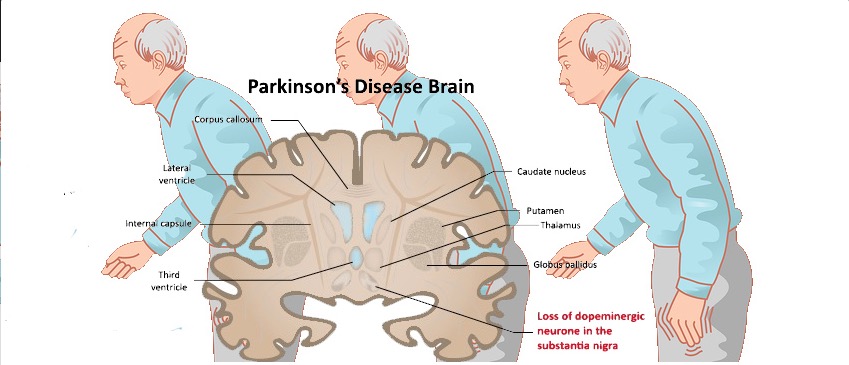
帕金森病(Parkinson's disease,PD)是老年人的一种进行性神经退行性疾病,表现为典型的运动症状,如静止性震颤、僵直和缓行性运动,以及非运动症状。根据主要的运动症状,PD可分为运动性强直(AR)亚型和震颤为主(TD)亚型。临床证据表明,不同的PD亚型有不同的临床病程和预后。事实上,相对于TD亚型,AR亚型往往临床进展更快,发展为痴呆和其他精神疾病(如抑郁症)的风险更高,这说明亚型之间的神经基础不同。
神经影像学研究已经记录了TD和AR亚型中不同的脑部改变模式。值得注意的是,这两个亚型有明显的小脑形态学改变,而其皮质形态学仍基本未被研究。皮质褶皱化(cortical gyrification)是大脑皮层最突出的形态学特征,已被证明在PD患者中发生了改变。但仍有一个问题是,这两种亚型是否与不同的皮质褶皱变化模式有关。
目前认为皮质褶皱化由潜在的白质(WM)张力所驱动,皮质褶皱变化是否与每个亚型的WM异常有关,值得探究。
最近,中国电子科技大学的Xie Tang探究了:
(1)与健康对照组(HCs)相比,AR和TD亚型的皮层褶皱化;
(2)每个亚型的皮层褶皱化是否与WM异常有关。
他们纳入了64名AR亚型患者、26名TD亚型患者和56名健康对照组(HCs)。为每位参与者获取了高分辨率结构和扩散加权图像。并计算了局部褶皱化指数(LGI)和分数各向异性(FA),以确定AR和TD亚型的皮质褶皱化和WM微结构变化。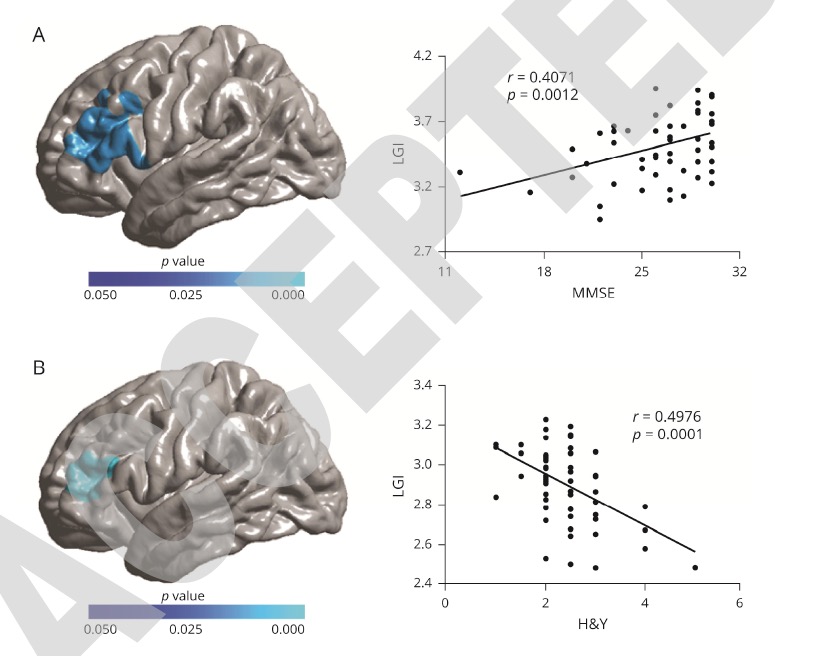
他们发现,与HCs相比,AR亚型患者的腹前、腹后、下和上顶叶、中和上额/颞叶、前和后扣带、眶前叶、上边缘、楔前叶和部分视皮质的LGI降低,皮质脊髓束、下和上纵束、下前枕束、前丘脑放射的FA降低。
AR亚型的LGI和FA的减少是紧密耦合的。左额下回和中额回的LGI与AR亚型患者的MMSE评分和Hoehn和Yahr评分(评估帕金森进展)相关。与AR亚型和HCs患者相比,TD亚型患者的LGI和FA无明显变化。
这个研究的重要意义在于,发现了PD的皮质褶皱化是运动表型特异性的,这可能是由关联的WM微结构异常所介导。
Neurology Mar 2021, 10.1212/WNL.0000000000011894; DOI: 10.1212/WNL.0000000000011894
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#中国原创研究#
44
#Neurol#
22
#表型#
38
#大脑皮层#
29