Modern Pathology:人工智能辅助能够显著改善病例学家对前列腺活检的格林森分级
2020-08-20 AlexYang MedSci原创
格林森评分是前列腺癌患者最重要的预后标记,但是受观察者的影响很大。基于深度学习的人工智能(AI)系统在格林森分级中能够达到病理学家水平。然而,该系统的表现性能在人工制品,异体组织或者其他异常存在的情况
格林森评分是前列腺癌患者最重要的预后标记,但是受观察者的影响很大。基于深度学习的人工智能(AI)系统在格林森分级中能够达到病理学家水平。然而,该系统的表现性能在人工制品,异体组织或者其他异常存在的情况下会有所降低。病理学家将他们的经验与AI系统的反馈结果整合能够产生协同效果,会优于单独的病理学家结果和系统结果。尽管人工智能非常火热,关于上述问题的文献却非常有限。

最近,有研究人员调查了AI协助分级前列腺活检的价值情况。研究共包括了14名观察者和160例活检样本,包括了AI协助和不协助两种情况。研究发现,使用AI时,专家组与专家参考标准的一致性显著增加(二次加权Cohen's kappa 0.799 vs. 0.872;p=0.019)。在一个包括87个病例的外部验证集中,专家组结果与国际前列腺病例专家组结果的一致性显著增加(二次加权Cohen's kappa 0.733 vs. 0.786; p=0.003)。在上述两个试验中,在小组水平上AI协助病理学家的表现要由于无协助的病理学家和单独的AI系统。
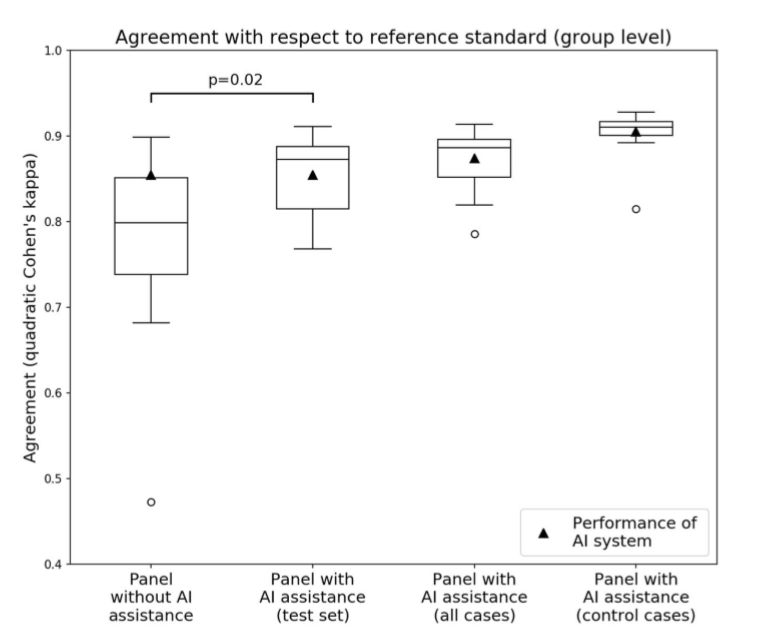
有无AI协助时的专家组表现
最后,研究人员指出,他们的结果表明了AI系统在格林森分级上的潜力,更重要的是,病理学家-AI系统能够产生有益的协同作用。
原始出处:
Wouter Bulten, Maschenka Balkenhol, Jean-Joël Awoumou Belinga et al. Artificial intelligence assistance significantly improves Gleason grading of prostate biopsies by pathologists. Modern Pathology . August 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#前列腺活检#
42
#Pathol#
32
#活检#
34
牛,人工智能!
78