JACC:PCI术后自发性出血和心肌梗死增加患者的远期死亡率
2015-05-11 张旭栋 MedSci原创
美国加州大学旧金山分校Dhruv S. Kazi博士等人,研究了PCI术后患者出血和心肌梗死与远期死亡率之间的关联性,其研究成果发表在4月份Journal of the American College of Cardiology期刊上。 背景: 经皮冠状动脉介入治疗(PCI)后使用血小板抑制剂能够降低心肌梗死(MI)的风险,但同时也会增加患者出血风险。PCI术后住院期间MI和出血与远
美国加州大学旧金山分校Dhruv S. Kazi博士等人,研究了PCI术后患者出血和心肌梗死与远期死亡率之间的关联性,其研究成果发表在4月份Journal of the American College of Cardiology期刊上。
背景:
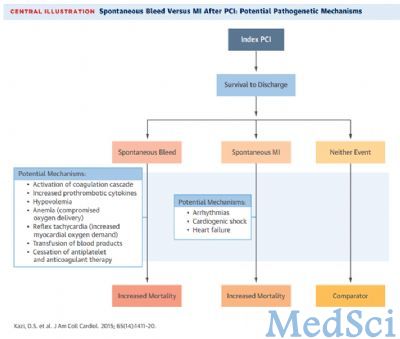
经皮冠状动脉介入治疗(PCI)后使用血小板抑制剂能够降低心肌梗死(MI)的风险,但同时也会增加患者出血风险。PCI术后住院期间MI和出血与远期预后呈负相关。出院后自发性出血对远期死亡率的影响依旧未知。
目的:
本研究旨在探讨PCI术后自发性大出血或心肌梗死与远期死亡率之间的关联。
方法:
研究回顾了综合医疗服务体系中1996年至2008年行PCI术的患者(≥30岁)。对人口统计,合并症,围手术期事件和远期药物暴露进行了调整,并使用Cox回归分析研究了自发性出血和MI与全因死亡率之间的关联。
结果:
32906例患者(PCI术后生存的患者)中,7至365天出院后,530例患者有出血发生,991例患者发生心肌梗死。平均随访4.42年后,有4,048例患者死亡。自发出血(9.5%)和心肌梗死(7.6%)患者的年死亡率比未发生出血和心肌梗死的患者高(2.6%)。出血风险能够增加年死亡率(调整后风险比HR:1.61,95%置信区间1.30〜2.00),MI同样也能增加患者年死亡率(调整后风险比HR:1.91; 95%可信区间:1.62至2.25 )。远期使用抗血小板药物后,出血与死亡率仍保持高相关性。
结论:
PCI术后自发性出血能够增加患者的远期死亡率,与随访心肌梗死死亡率相媲美。这项对于个体化抗血小板治疗的疗效和安全性研究,为患者远期血栓和出血风险中使用抗血小板治疗提供了论据。
原文出处:
Kazi DS, Leong TK, Chang TI, Solomon MD, Hlatky MA, Go AS. Association of spontaneous bleeding and myocardial infarction with long-term mortality after percutaneous coronary intervention. Journal of the American College of Cardiology. 2015;65(14):1411-20.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PCI术#
22
#JACC#
33
出血……看大小
96
#ACC#
30
#PCI术后#
22
#自发性#
27