Stroke:边缘带梗死和侧枝血流受损者应该置入颅内支架?
2019-03-08 杨中华 脑血管病及重症文献导读
颅内动脉粥样硬化狭窄(Intracranial atherosclerotic arterial stenosis,ICAS)是缺血性卒中的常见病因,与高复发卒中的风险有关。
颅内动脉粥样硬化狭窄(Intracranial atherosclerotic arterial stenosis,ICAS)是缺血性卒中的常见病因,与高复发卒中的风险有关。SAMMPRIS 试验显示对于近期70-99% ICAS所致 TIA 或非致残性卒中患者,单独积极内科治疗优于经皮腔内成形术/支架联合最佳内科治疗。尽管积极内科治疗具有优势,在平均32.4个月的随访中内科治疗组仍然有15%的患者发生了主要终点事件。
以前 SAMMPRIS 试验内科治疗组的分析显示因卒中纳入试验(不是 TIA)与卒中复发强烈相关。然而,这项分析并未验乞卒中(qualifying strokes)的梗死模式类型与预后之间的关系。以前的研究发现梗死模式常与卒中的特殊机制(比如栓塞、血流动力学衰竭、穿支)有关,与卒中复发风险有关。
2019年1月来自美国的 Ashley M. Wabnitz 等在 Stroke 上公布了他们的研究结果,他们利用 SAMMPRIS 试验内科治疗组的患者,验乞了梗死模式和卒中复发风险之间的关系,特别着眼于患者血流动力学不足的影像学标志(边缘带区域梗死和侧枝循环受损)。
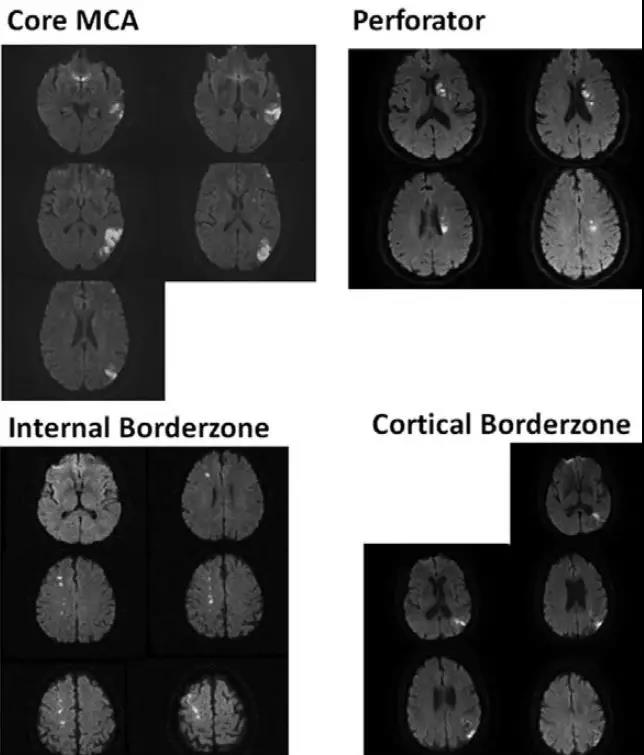
该事后分析纳入的患者为 SAMMPRIS 试验中因脑梗死纳入研究的内科治疗组患者,这些患者的梗死位于狭窄的MCA 或颈内动脉颅内段供血区。梗死分类为:内边缘带区,皮层边缘带区,核心 MCA 区或穿通动脉区;按照标准量表(American Society of Interventional and Therapeutic Neuroradiology/Society of Interventional Radiology)评价侧枝血流。
共101例患者,边缘带梗死者该区域复发性卒中的比例为26.4%,核心 MCA 梗死者为8.3%,穿通动脉梗死者为12.5%(三组比较 P = 0.14,边缘带 vs 非边缘带 P = 0.52)。在评价了侧枝血流的82例患者中,70%的边缘带梗死、37%的核心MCA 梗死和55%的穿通动脉梗死存在狭窄远端侧枝血流受损(P = 0.049)。边缘带梗死和侧枝血流受损者的卒中复发风险最高(37%)。
最终作者认为对于采取内科治疗的颅内动脉狭窄的患者,边缘带梗死和侧枝血流受损者处于高卒中复发风险之中。
原始出处:Ashley M. Wabnitz, Colin P. Derdeyn, David J. Fiorella, et al. Hemodynamic Markers in the Anterior Circulation as Predictors of Recurrent Stroke in Patients With Intracranial Stenosis. Stroke. 11 Dec 2018
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






谢谢分享,学习了
57
学习谢谢分享
54
好好好好好好
56