Chest:运动训练可提高肺动脉高压患者的心肺功能和生活质量
2013-05-09 Chest dxy
肺动脉高压(PH)对患者从事体力活动的能力及患者的寿命有很大的危害。针对这一情况,来自美国国家卫生研究院康复医学部的Leighton Chan等人对世界卫生组织的1组PH患者进行了前沿性研究,该研究主要探讨有氧运动对PH患者的心肺功能及生活质量的影响,结果发表于2013年2月1日的美国胸科杂志(Chest)上。结果表明运动训练可以改善肺动脉高压患者的心肺功能及生活质量。该研究中患者被随机分为为期1
肺动脉高压(PH)对患者从事体力活动的能力及患者的寿命有很大的危害。针对这一情况,来自美国国家卫生研究院康复医学部的Leighton Chan等人对世界卫生组织的1组PH患者进行了前沿性研究,该研究主要探讨有氧运动对PH患者的心肺功能及生活质量的影响,结果发表于2013年2月1日的美国胸科杂志(Chest)上。结果表明运动训练可以改善肺动脉高压患者的心肺功能及生活质量。
该研究中患者被随机分为为期10周的教育组(EDU)和教育-运动联合组(EXE)。运动训练计划包括24-30个阶段,每个阶段的主要内容是在保持70%-80%的心率储备指数的情况下进行30-45分钟的跑步机行走训练。结果变量包括:6分钟步行实验(6MWT)的距离变化,运动耐受的极限时间,心肺运动实验中的最大功率;生活质量的评估措施包括:2版健康生活质量调查简表(SF-36v2),剑桥肺动脉高压结果回馈表(CAMPHOR)。
研究结果数据以平均值±标准差来表示。23名女性患者(年龄54±11岁;体重指数BMI 31±7kg/m2)被随机分为EDU组(n=13)和EXE组(n=10)。经过10周的实验干预,EXE组结果:6分钟步行实验的距离变化(56 ±45m;P =0.002<0 .050),运动耐受的极限时间(1.9±1.3min;P=0.001<0.050),最大功率(26±23W;P=0.004<0.050),结果表明EXE组在6分钟步行实验的距离变化、运动耐受的极限时间、最大功率方面均有显著差异。生活质量评估方面EXE组在2版健康生活质量调查简表(SF-36v2)的8项评分项目中有6项的得分有显著差异,剑桥肺动脉高压结果回馈表(CAMPHOR)的6项评分项目中有5项的得分有显著差异。而EDU组的结果变量及生活质量评估均无显著差异。全组实验对象无任何有害结果。
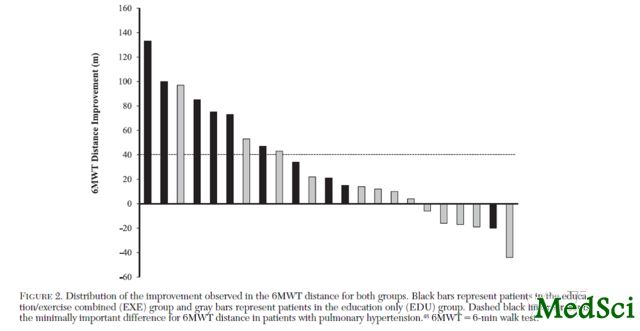
图为两组在6分钟步行实验中的距离提高的分布图,黑条为EXE组,白条为EDU组。虚线代表6分钟步行实验中的最小显著区别
经过10周的步行训练EXE组在在6分钟步行实验的距离,运动耐受的极限时间、最大功率方面均有显著差异,表明运动训练可以提高患者的体力活动能力及心肺功能,而生活质量评估方面EXE组在2版健康生活质量调查简表(SF-36v2)的8项评分项目中有6项的得分有显著差异,剑桥肺动脉高压结果回馈表(CAMPHOR)的6项评分项目中有5项的得分有显著差异。表明运动训练也有助于改善患者的生活质量。所以运动训练可以改善肺动脉高压患者的心肺功能及生活质量。
与肺动脉相关的拓展阅读:
- JAMA IM:1/3肺动脉高压往往被错误诊断
- Circulation:伊马替尼治疗肺动脉高压风险获益并存
- Circulation:曲罗尼尔有望成为肺动脉高压一线治疗药物
- AM J RESP CRIT CARE:社会经济地位与肺动脉高压全因死亡率呈负相关
- Circulation:间充质干细胞分泌外染色体抑制缺氧性肺动脉高压
- IJBCB:TGFβ1/15-LO通路可能成为肺动脉高压新靶点 更多信息请点击:有关肺动脉更多资讯

Benefits of Intensive Treadmill Exercise Training on Cardiorespiratory Function and Quality of Life in Patients With Pulmonary HypertensionExercise Training in Pulmonary Hypertension
Background
Pulmonary hypertension (PH) restricts the ability to engage in physical activity and decreases longevity. We examined the impact of aerobic exercise training on function and quality of life in patients with World Health Organization group 1 PH.
Methods
Patients were randomized to a 10-week education only (EDU) or education/exercise combined (EXE) group. The exercise program consisted of 24-30 sessions of treadmill walking for 30-45 min per session at 70% to 80% of heart rate reserve. Outcome variables included changes in 6-min walk test (6MWT) distance, time to exercise intolerance, peak work rate (WR) from a cardiopulmonary treadmill test, and quality-of-life measures, including the Short Form Health Survey, version 2 (SF-36v2) and Cambridge Pulmonary Hypertension Outcome Review (CAMPHOR).
Results
Data are presented as mean ± SD. Twenty-three women (age, 54 ± 11 years; BMI, 31 ± 7 kg/m2) were randomized to the EDU (n = 13) or EXE (n = 10) groups. Following 10 weeks of intervention, patients in the EXE group demonstrated an improvement in 6MWT distance (56 ± 45 m; P = .002), increased time to exercise intolerance (1.9 ± 1.3 min; P = .001), and peak WR (26 ± 23 W; P = .004). Additionally, the EXE group scored significantly (P < .050) better on six of the eight scales on SF-36v2, and five of the six scales on CAMPHOR. In contrast, no significant improvement was observed for any of the outcome measures following EDU. No adverse events were noted in either group.
Conclusion
Ten weeks of brisk treadmill walking improved 6MWT distance, cardiorespiratory function, and patient-reported quality of life in female patients with group 1 PH.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#动脉高压#
39
#心肺#
37
#EST#
0
#肺动脉高压患者#
46
#运动训练#
29
#Chest#
29
#心肺功能#
30