Virulence:IFNL4基因型影响男男性行为者的HIV-1血清转换率
2022-06-22 从医路漫漫 MedSci原创
G-IFNL4基因(功能变异)与治疗初期和无症状个体中较低的CD4+淋巴细胞、CD4+/CD8+淋巴细胞比率正常化和较高比例的单纯CD8+T细胞以及病毒抑制后较低的CD4+效应记忆细胞相关。
背景:全基因组关联研究发现,IFNL3(IL28B)上游的遗传变异是预测丙型肝炎病毒感染的自发和干扰素-α/利巴韦林治疗依赖的治愈的有效生物标记物。与这些表型相关的最显著的SNP是位于IFNL3上游的rs12979860。后来,这个功能变体被定位在一个靠近IFNL3的新基因中,命名为IFNL4。该变异(Rs368234815)是一种插入-缺失多态(Indel),具有功能性的IFNL4编码等位基因(G)和零等位基因(TT),导致移码突变,没有IFNL4蛋白。与功能变异体不同,rs12979860位于内含子内,两个变异体之间相隔418个碱基对。INFL4在体外显示出强大的抗病毒活性,因此令人困惑的是,该蛋白的缺陷可以增强对几种传染病的抵抗力。IFNL4基因是否会改变艾滋病毒携带者的免疫状态仍然存在争议,报道的结果相互矛盾。
G-IFNL4基因(功能变异)与治疗初期和无症状个体中较低的CD4+淋巴细胞、CD4+/CD8+淋巴细胞比率正常化和较高比例的单纯CD8+T细胞以及病毒抑制后较低的CD4+效应记忆细胞相关。相反,IFNL4基因与即使长期病毒抑制也无法恢复CD4T细胞水平无关。此外,G-IFNL4基因与巨细胞病毒视网膜炎、肺结核和肺孢子虫肺炎的高患病率有关。
Martin等人。研究了INFL4对HIV-1阳性与非HIV-1感染者的易感性的影响。来自美国的高度暴露的未感染的人,包括欧洲和非洲血统的个人。他们发现,在高度暴露于血清阴性的人中,没有发现与保护有关。在北非人群中也发现了类似的结果。然而,这些研究没有对位于IFNL4开放阅读框架中的功能性Indel进行基因分型,而是对第一内含子中的另一个SNP进行了基因分型。这一事实具有重要的统计学意义,因为这两种变异在欧洲人和亚洲人中处于完全连锁不平衡状态,但在非洲血统的个体中不存在。在西班牙和爱沙尼亚的静脉注射吸毒者中,发现IFNL4的零等位基因对HIV-1感染具有高度的保护作用。此外,Jaimes-Beral等人。在通过与感染艾滋病毒-1的伴侣进行异性接触而有感染风险的高暴露血清阴性个人中,发现了同样的趋势。
目的:这项研究旨在确证或反驳在男男性行为人群(MSM)中IFNL4无效等位基因与HIV-1易感性之间的联系。
方法:在一项针对HIV-1的预防性疫苗试验中,对619名HIV-1血清阴性的男男性接触者进行了36个月的随访,评估了IFNL4无效基因型。其中,257人在此期间血清转化。构建了包括人口统计学和IFNL4基因型的逻辑回归模型。此外,还使用当前研究和其他欧洲人群的数据进行了荟萃分析。
结果:无效的IFNL4基因型与较低的HIV-1血清转换相关(校正OR = 0.4[95% CI:0.2–0.8],P = 0.008),与较长的血清转换时间相关(889天对938天,P= 0.01)。这些结果通过纳入其他欧洲人群数据的荟萃分析进行了验证,结果显示显性模型下的IFNL4无效基因型与较低的HIV-1感染概率显著相关(OR = 0.4[95% CI:0.3-0.6];p = 1.3×10E-5)。
表1 在Vax004临床试验的所有队列、疫苗接种者和安慰剂治疗受试者中INFL4基因型的基因型分布。
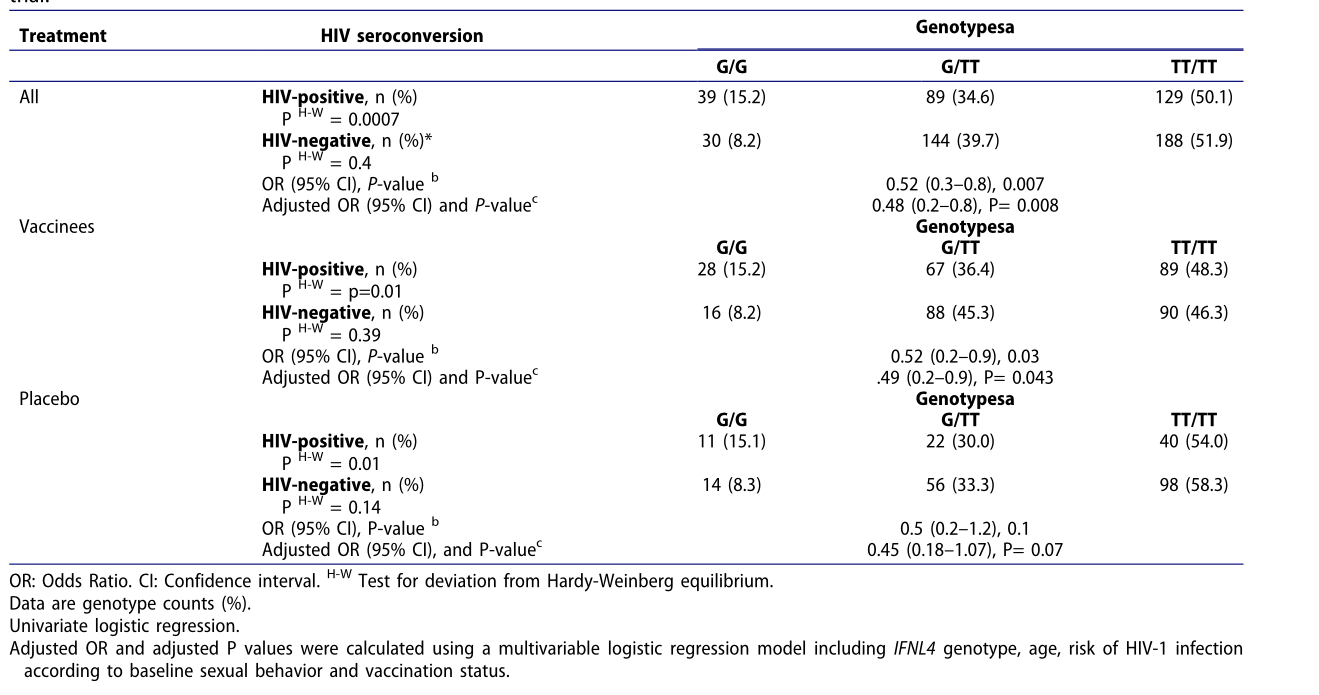

图1 根据IFNL4基因型的HIV-1血清转化率的卡普兰-迈耶图。通过对数秩检验(P=0.01),在rs368234815多态性的显性模型下比较存活曲线(TT+GT对GG)。g是功能性IFNL4等位基因。
表2 HIV-1血清转化的预测因子
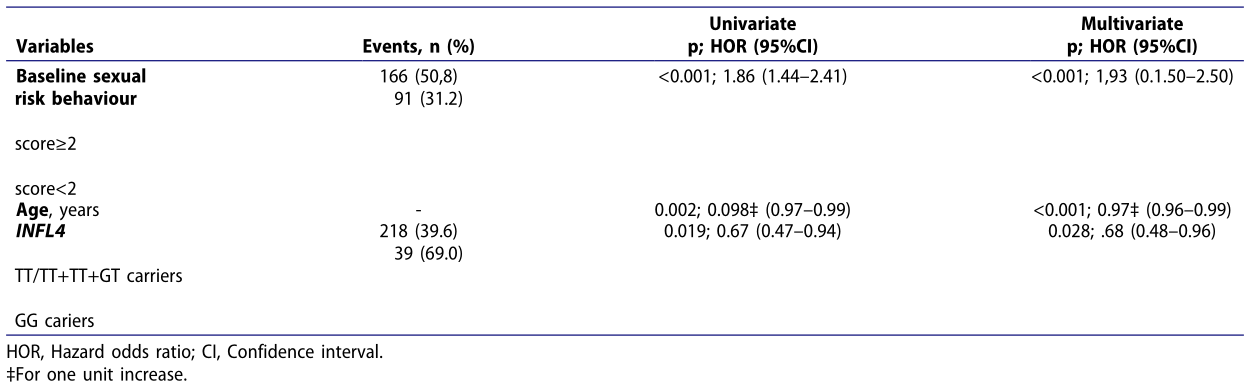
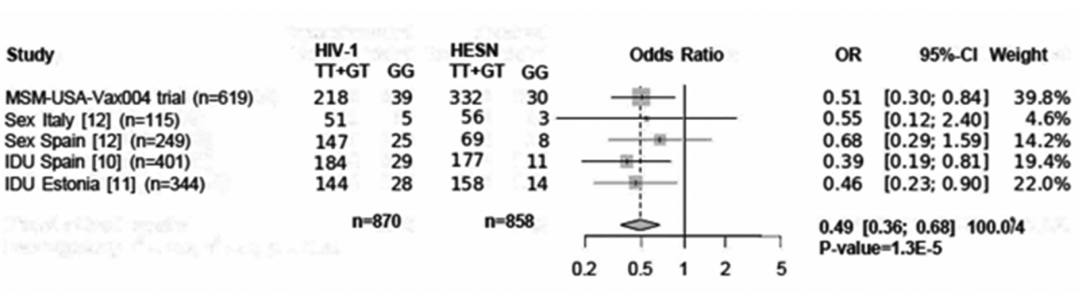
图2 来自西班牙和爱沙尼亚(https://metagenyo.genyo.es/)的男男性行为者(MSM-USA-Vax004试验)、血清不一致夫妇(Sex Italy和Spain)和静脉注射毒品使用者(IDU)人群的荟萃分析森林图。优势比(OR)和95%置信区间(95%-CI)和固定效应荟萃分析。保护性等位基因的显性模型的p = 1.3 x 10-5(G/G对TT/TT+TT/G)。
结论:这项研究(1)在一个独立的MSM人群中再次研究了IFNL4和先天HIV-1之间的关系,( 2)确定了IFNL4无效等位基因在欧洲人群中预防HIV感染的作用。
原文出处:Meza G, Galián F, Jaimes-Bernal C,et al.IFNL4 genotype influences the rate of HIV-1 seroconversion in men who have sex with men.Virulence 2022 12;13(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#基因型#
47
#性行为#
40
#男男性行为#
41
#IFN#
49
学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习
46