BJU Int:肾细胞癌中的癌症相关成纤维细胞对预后和抗血管生成疗法的影响研究
2021-06-27 AlexYang MedSci原创
肾癌是男性中第六大最常见的癌症,女性中第九大最常见的癌症。 在发病率和死亡率方面,它是第三大泌尿科癌症。最近,肾癌的管理和对其生物学的理解已经取得了很大的进展。确定了不同的组织学亚型,其特征是不同的遗
肾癌是男性中第六大最常见的癌症,女性中第九大最常见的癌症。 在发病率和死亡率方面,它是第三大泌尿科癌症。最近,肾癌的管理和对其生物学的理解已经取得了很大的进展。确定了不同的组织学亚型,其特征是不同的遗传和分子改变,并对应于不同的致癌途径,可通过到靶向治疗抑制。

世界卫生组织在2016年修订的分类中区分了13种肾细胞癌(RCC)的亚型。其中,透明细胞肾细胞癌(ccRCC)是最常见的组织学亚型(占所有肾癌的70-75%)。近期,有研究人员调查了癌症相关成纤维细胞(CAFs)在透明细胞肾细胞癌(ccRCC)中对肿瘤侵袭性、转移发展和对抗血管生成治疗(VEGFR-酪氨酸激酶抑制剂,VEGFR-TKI)的抗性作用。
研究涉及三个不同的、独立的ccRCC患者队列的组织样本。通过转录特征分别调查了CAFs和肿瘤淋巴管的生成,调查了与肿瘤的发展和预后的关联。在ccRCC细胞与CAFs的共同培养中,分析了CAFs对肿瘤细胞迁移和VEGFR-TKI抗性的影响。
结果表明,VEGFR-TKI明显增加了肿瘤中CAFs的数量。在相同的ccRCC患者群体中,肿瘤内CAFs的比例与较短的无病和总生存期相关。CAFs的存在也与淋巴管生成和淋巴结转移相关。CAFs增加了肿瘤细胞的迁移并降低了VEGFR-TKI依赖的细胞毒性作用。
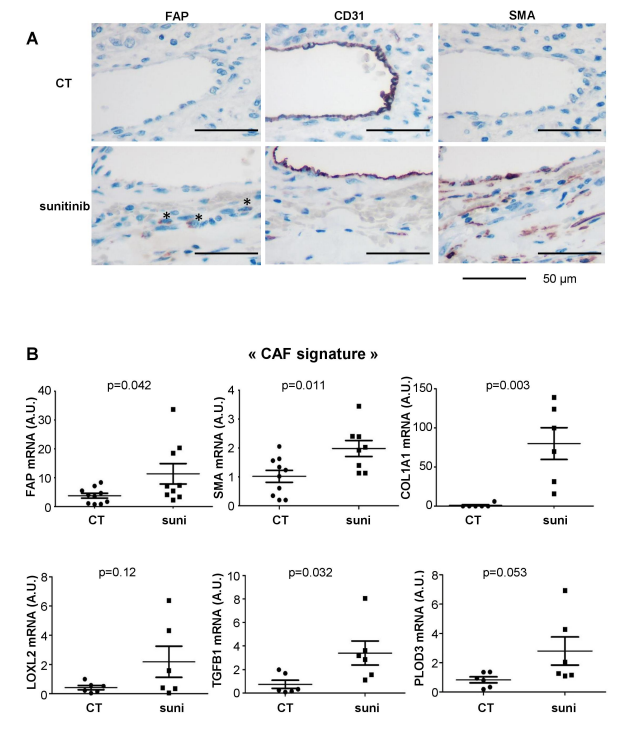
Sunitinib能够增加CAFs水平
综上所述,他们的研究结果表明,VEGFR-TKI促进了CAFs的发展,CAFs有利于ccRCC的肿瘤侵袭性、转移性扩散和抵抗治疗。CAFs可以代表一个新的治疗目标来对抗ccRCC的治疗抗性。靶向CAF和免疫疗法的结合正在成为许多类型实体瘤的有效治疗方法。
原始出处:
Damien Ambrosetti, Michael Coutts, Charlotte Paoli et al. Cancer associated fibroblasts in Renal Cell Carcinoma: implication in prognosis and resistance to antiangiogenic therapy. BJU Int. Jun 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#癌症相关成纤维细胞#
38
#抗血管#
0
#癌症相关#
34
#细胞癌#
38
#成纤维细胞#
42
#纤维细胞#
33
#抗血管生成#
46