Blood:采用CAR T细胞疗法(liso-cel)治疗复发性/难治性CLL/SLL
2021-11-13 Nebula MedSci原创
总缓解率高达82%,其中45%的为完全缓解
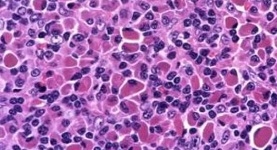
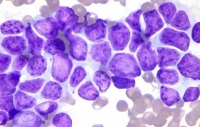
目前,新确诊的和复发性或难治性慢性淋巴细胞白血病(CLL)或小淋巴细胞淋巴瘤(SLL)患者多采用Bruton酪氨酸激酶抑制剂(BTKi)和维奈托克(venetoclax)治疗。但是大多数患者最终会对这些疗法产生耐药性,这凸显了对新型有效疗法的需求。
近日,国际著名期刊《血液》上发表了一项多中心、开放标签的1/2期TRANSCEND CLL 004 (NCT03331198) 研究的1期剂量递增阶段的研究结果,该研究探索了采用一种自体 CD19 靶向嵌合抗原受体 (CAR) T 细胞疗法,lisocabtagene maraleucel (liso-cel),治疗复发性/难治性 CLL/SLL 的潜在可能。
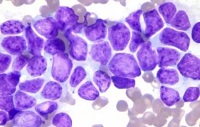
在该研究中,既往治疗过两三次以上(包括BTKi)的标准或高风险特征的 CLL/SLL 患者接受两种剂量的 liso-cel(50×106或100×106个CAR+ T细胞)。主要终点包括安全性和确定推荐的剂量;探索性终点为抗肿瘤活性。评估骨髓和血液中的最小残留病灶(MRD)。
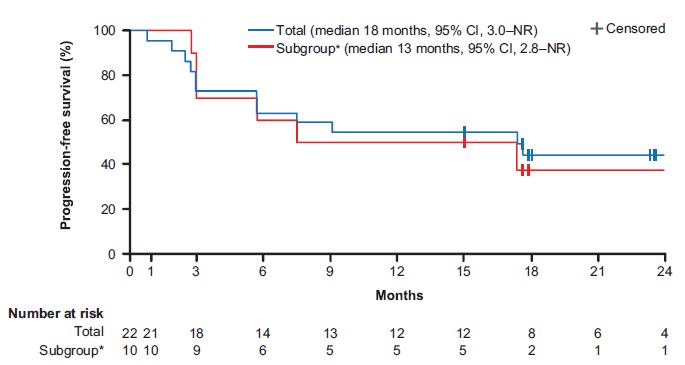
无进展生存期
共招募了25位患者,其中23位接受了 liso-cel,被纳入安全性分析。受试患者的中位既往治疗次数为4次(范围 2-11次;都接受过依鲁替尼治疗,65%的接受过维奈托克治疗)。83%的患者有高风险特征,携带TP53突变或del(17p)。
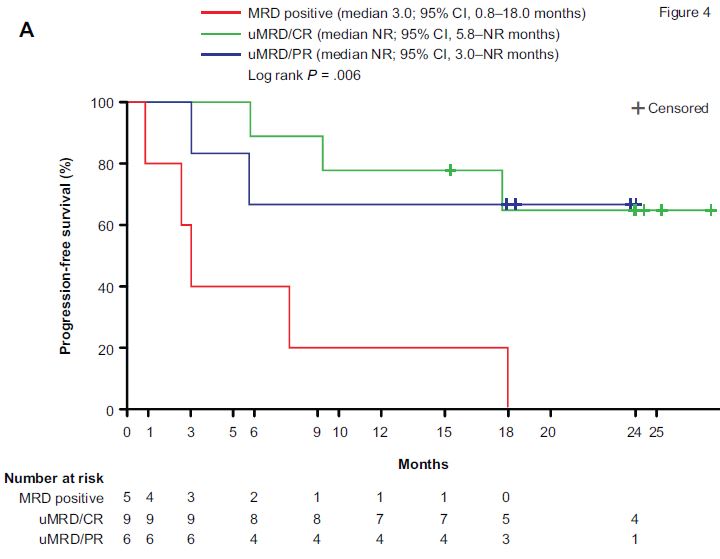
根据MRD状态分组的患者的无进展生存期
74%的患者发生了细胞因子释放综合征(9%的是3级),39%的患者发生了神经事件(22%的3/4级)。在22位可评估疗效的患者中,总缓解率高达82%,其中45%的为完全缓解。在20位 MRD 可评估的患者中,分别有75%和65%的患者在血液和骨髓中检测不到MRD。此外,两种剂量水平的疗效和安全性相似。
该研究第2阶段 liso-cel 的剂量水平为 100×106个CAR+ T细胞。
原始出处:
Tanya Siddiqi, et al. Phase 1 TRANSCEND CLL 004 study of lisocabtagene maraleucel in patients with relapsed/refractory CLL or SLL. Blood .2021011895. https://doi.org/10.1182/blood.2021011895
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#CEL#
31
#T细胞疗法#
43
#难治性#
27
#liso-cel#
0
#CLL/SLL#
40
#复发性#
22
实用
53