Lancet Neurol:宣武医院贾建平团队全方面论述中国痴呆现状并提出痴呆防控方略
2019-09-09 佚名 中华医学信息导报
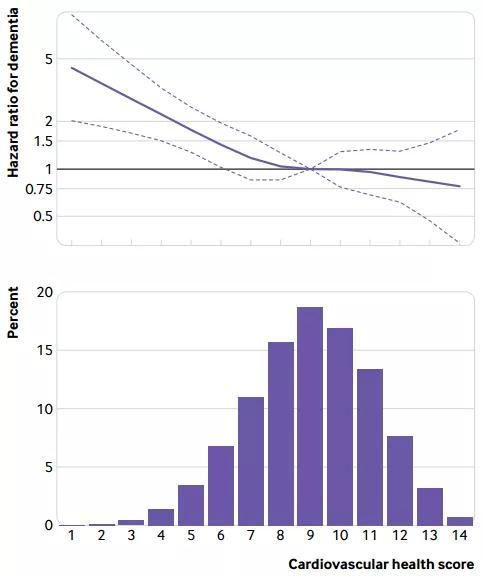
中国目前是世界上人口最多的国家(14亿),老年人口占17.9%,已经逐步进入老龄化社会。老年人口的增多导致老年神经系统变性疾病尤其是痴呆的增多,目前推算有痴呆患者超过1000万,MCI患者3100万,卒中后痴呆患者950万,总计5000多万痴呆与认知障碍人群。面对如此庞大的痴呆和认知障碍患病人群,一方面我们意识到目前相应的医疗服务和护理还不能满足患者的需求,另一方面我们要反思痴呆患病人群连年增
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Lancet#
36
#宣武医院#
40
#Neurol#
30
学习了,,谢谢分享
79
谢谢了,学习
94
好
82
老年人痴呆何药可用??
59