Haematol:接受尼罗替尼一线治疗的慢性粒细胞白血病患者的无治疗缓解:10 年随访研究
2022-04-16 网络 网络
在 CP-CML 中使用 NIL 前线可以在相关数量的患者中诱导稳定的 TFR,尽管心血管毒性仍然值得关注。
尼洛替尼(NIL)是一种酪氨酸激酶抑制剂(TKI),最初被证明对慢性期(CP)慢性髓系白血病(CML)耐药或不耐受的患者有效,每日两次400mg,耐受性良好。
此次报告一项10年随访研究,该研究招募了 73 名新诊断为慢性期的成年患者(中位年龄 51 岁,范围 18-83) (CP)-慢性粒细胞白血病 (CML) 以研究尼罗替尼 (NIL) 一线治疗的疗效和毒性。
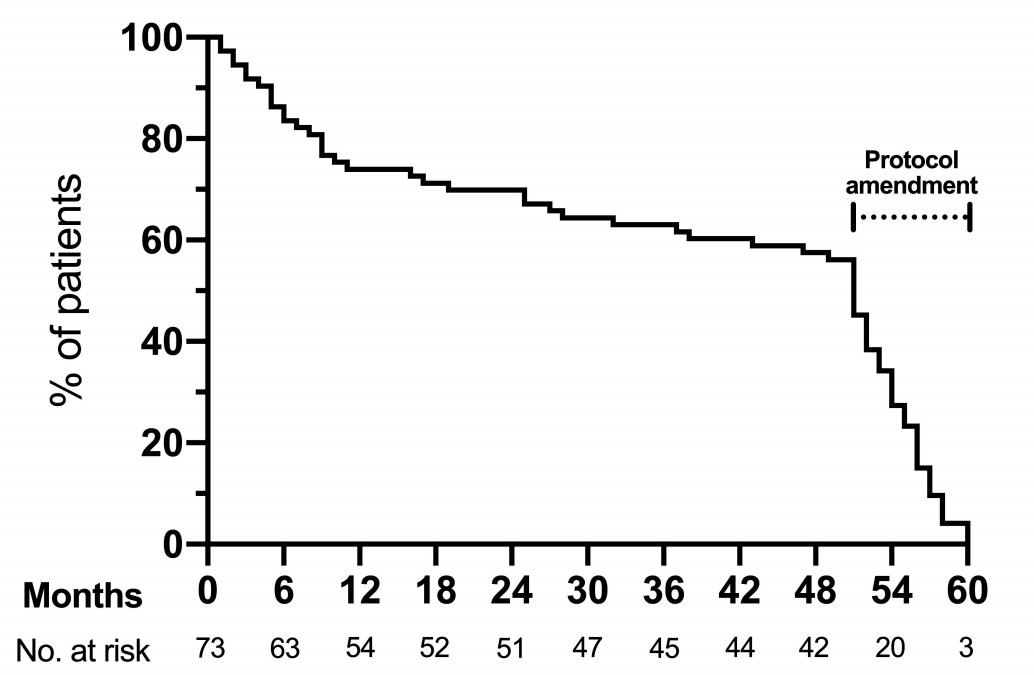
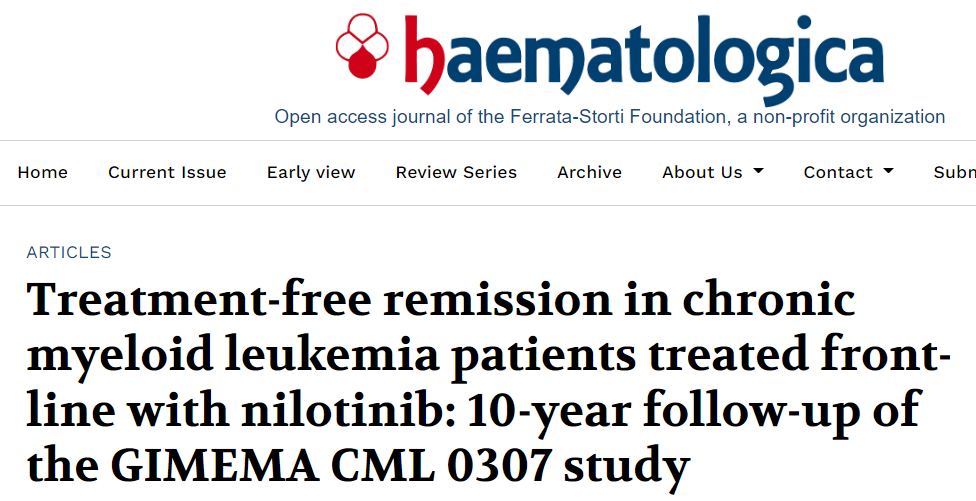
图1:在研究的前5年,NIL400mg的治疗时间。2007年至2008年期间,所有患者开始注射新生儿注射,剂量为400mg,每日两次。授权后在意大利2011年11月的零的剂量300毫克每日两次的一线治疗,GIMEMA协议修改,这样所有患者仍然接受剂量400毫克每日两次减少到300毫克每日两次到2012年9月。NIL400mg的中位持续时间为51个月(IQR:25-56个月)。
尼罗替尼初始剂量为 400 毫克,每日两次;一旦该剂量获得批准和登记,剂量就减少到每天两次 300 毫克。10年总生存率和无进展生存率为94.5%。在最后一次接触时,36 名 (49.3%) 患者继续 NIL(22 名患者每天两次 300 mg,14 名低剂量),18 名(24.7%)患者处于无治疗缓解(TFR),14 名(19.2%)正在接受其他酪氨酸激酶抑制剂治疗,4 名(5.5%)患者死亡。
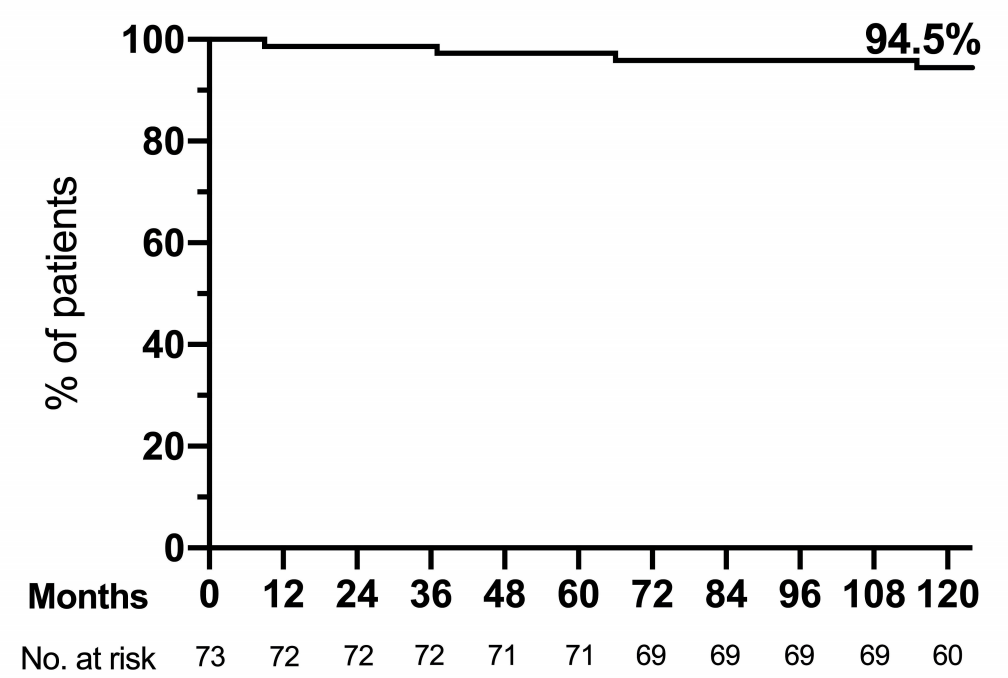
图2:10年总生存率
10 年主要 (MMR) 和深度 (MR4) 分子反应率分别为 96% 和 83%。MMR 和 MR4 的中位时间分别为 6 个月和 18 个月。NIL 治疗的中位持续时间为 88 个月后,24 名 (32.9%) 患者在稳定的深层分子反应期间停止了 NIL。
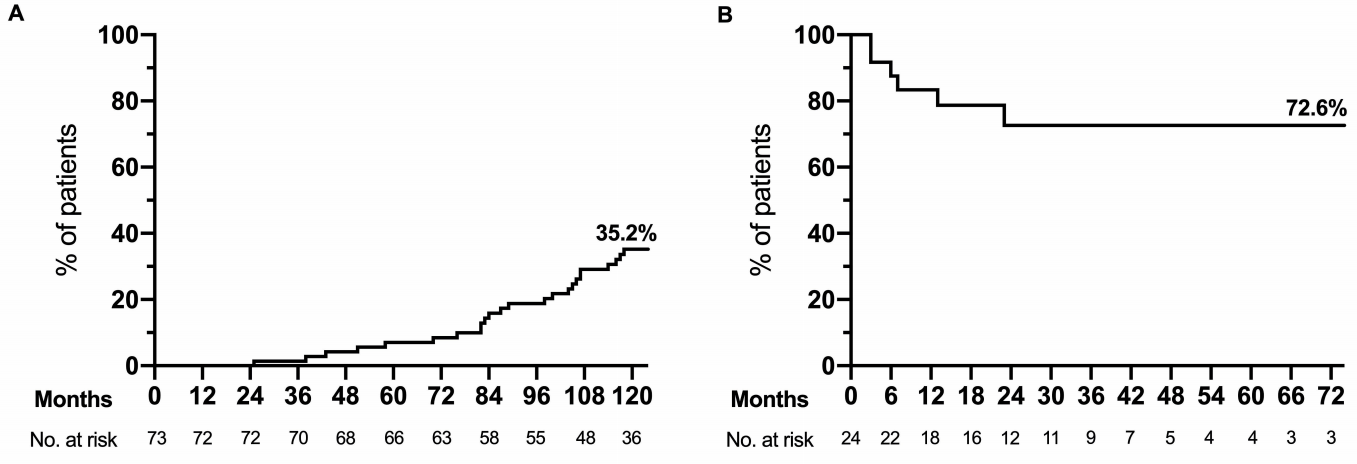
图3:无治疗缓解。a.TFR尝试的累积发生率。73例患者中有24例在DMR稳定时尝试了TFR。 B. 24例稳定DMR停用NIL患者的无治疗生存。18例患者保持了TFR(17例DMR稳定,1例MMR稳定),6例患者失去了MMR,恢复了TKI治疗。
在这些患者中,估计的 2 年无治疗生存率为 72.6%。对所有入组患者计算的总 TFR 率为 24.7%(18/73 患者)。17 名患者 (23.3%),中位年龄为 69 岁,至少有一次动脉阻塞事件。
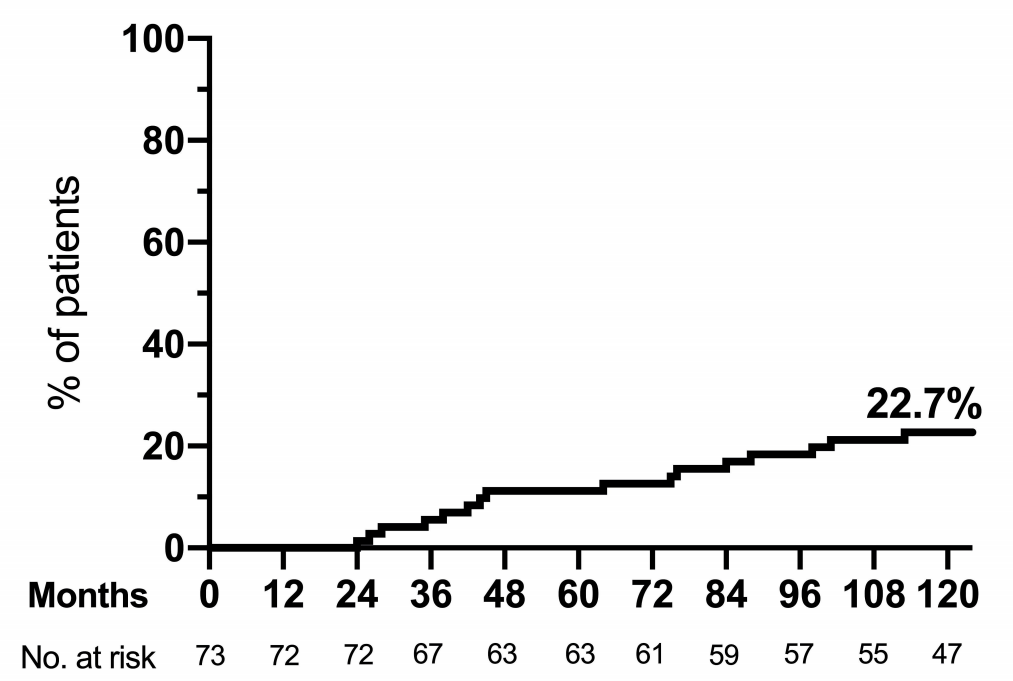
图4:动脉阻塞性事件的累积发生率。17例患者至少有动脉阻塞性事件。2名患者发生了多个事件(图中只报告了第一个事件)。
总的来说,该研究研究的长期结果表明,使用NIL一线能够在相关数量的患者中诱导稳定的TFR。然而,这种方法与AOEs是相关联的。通过根据年龄和个体心血管危险因素进行更准确的患者选择,以及随着时间的推移仔细调整剂量,能够获得TFR的CML患者的数量可能会增加,心血管并发症的数量可能会减少。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#HAE#
47
#随访研究#
44
#尼罗替尼#
44
坚持学习
0
#EMA#
33