Lancet Neurology:无症状颈动脉狭窄程度与卒中风险的关系:一项基于人群的队列研究、系统回顾和荟萃分析
2021-03-10 MedSci原创 MedSci原创
两项大型的随机对照试验证明,颈动脉内膜切除术对于近期有症状的颈动脉狭窄患者预防卒中的益处,其所观察到的益处在很大程度上取决于狭窄程度。
两项大型的随机对照试验证明,颈动脉内膜切除术对于近期有症状的颈动脉狭窄患者预防卒中的益处,其所观察到的益处在很大程度上取决于狭窄程度。在无症状性颈动脉狭窄为50%或更高的患者中进行的类似随机对照试验显示,与单纯药物治疗相比,动脉内膜切除术后卒中风险的降低更为温和。

然而,最近的队列研究表明,仅采用现代医学治疗可降低中风风险,这导致一些人质疑常规手术治疗的益处。从动脉内膜切除术治疗无症状颈动脉狭窄的三个关键临床试验中意外发现,药物治疗的卒中率以及干预的益处与狭窄的严重程度无关,这使得选择手术治疗的患者变得困难。本文主要研究目的是确定在接受现代医疗治疗的患者中,无症状狭窄程度与同侧卒中风险之间是否存在任何关联。
本研究是一项基于人群的前瞻性研究(Oxford血管研究,OxVasc)。在2002年4月1日至2017年4月1日期间,OxVasc中所有近期疑似短暂性缺血发作或中风的无症状颈动脉狭窄患者均纳入这些分析中。研究人员对其开始了现代医学治疗,并通过面对面随访(至2020年10月1日)确定了该队列中的同侧中风风险。不仅如此,作者团队还对所有发表的研究(1980年1月1日至2020年10月1日)进行了系统回顾和荟萃分析,这些研究报告了无症状颈动脉狭窄患者的同侧卒中风险。
2002年4月1日至2017年4月1日期间,共有2354名患者连续入组OxVasc,2178名患者接受了颈动脉成像,其中207名患者至少有一个颈动脉分叉出现50-99%的无症状狭窄(成像时的平均年龄: 77.5岁[SD10.3];88名[43%]女性)。5年同侧卒中风险随着狭窄程度的增加而增加;狭窄程度为70-99%的患者5年同侧卒中风险显著高于狭窄程度为50-69%的患者(53例患者中6例[14.6%;95%CI 3.5-25.7] VS 154例中0例;p<0.0001)。狭窄程度为80-99%的患者5年内发生同侧卒中的风险显著高于狭窄程度为50-79%的患者(34例患者中5例(18.3%;7.7-29.9%)VS 173例患者中1例(1.0%;0.0-2.9);p<0.0001)。
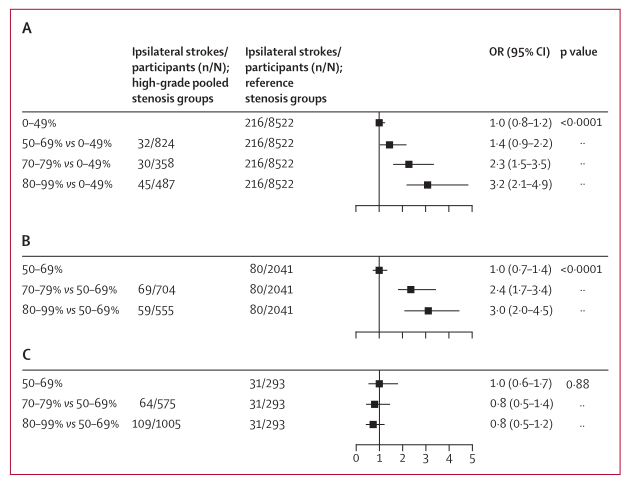
在系统回顾中确定的56项研究(包括13717名患者)中,其中23项提供了完全按无症状狭窄程度分层的同侧卒中风险数据(8419名患者)。卒中风险与同侧狭窄程度呈线性相关(p<0.0001);狭窄程度为70-99%的患者的卒中风险高于狭窄程度为50-69%的患者(3778例患者中有386例VS 3806例患者中有181例;比值比[OR]2.1[95%CI 1.7-2.5],p<0.0001;15项队列研究,3项临床试验)。狭窄率为80-99%的患者比狭窄率为50-79%的患者(727例患者中有77例狭窄VS 3272例患者中有167例狭窄;OR 2.5[1.8-3.5],p<0.0001;11项队列研究)。
总之,我们的研究结果证实了先前的报道,即无症状颈动脉狭窄远端卒中的风险在过去几十年中有所下降。然而,我们已经证明,在现代医学治疗中,高度狭窄患者的卒中风险仍然很高,这表明手术治疗的益处可能被低估。相反,在现代医学治疗中,中度狭窄患者的中风风险较低,这就对血管重建的益处提出了质疑。
Howard, Dominic P J et al. Risk of stroke in relation to degree of asymptomatic carotid stenosis: a population-based cohort study, systematic review, and meta-analysis.The Lancet Neurology, Volume 20, Issue 3, 193 - 202
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#无症状颈动脉狭窄#
40
#Neurol#
38
#颈动脉#
30
#荟萃#
26
#Lancet#
39
#风险的关系#
25
#荟萃分析#
27
#卒中风险#
32
#无症状#
31
#动脉狭窄#
32