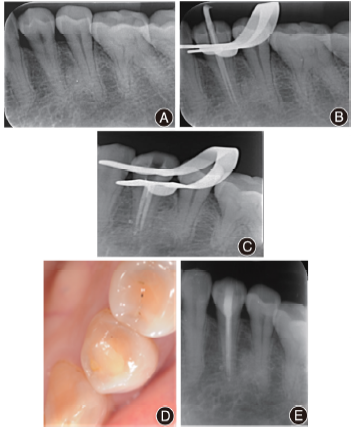
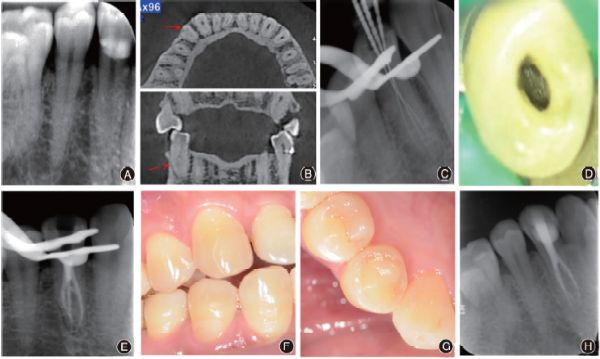
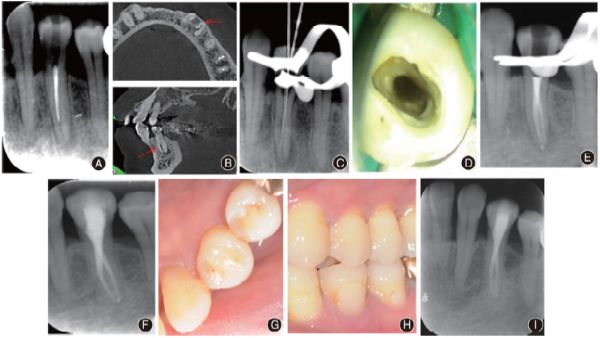
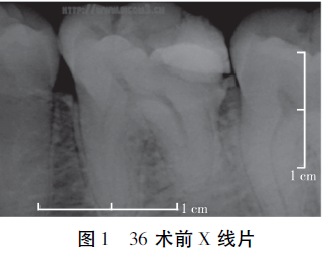
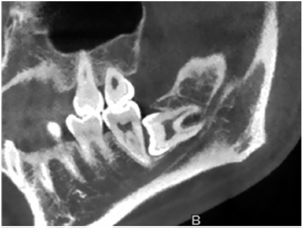
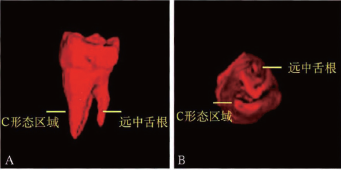
下颌**前磨牙变异根管的诊断和治疗4例
2019-11-19 王变红 侯本祥 北京口腔医学
根管治疗成功的关键在于准确认识根管系统的解剖形态,并对其进行完善预备成形、消毒以及三维充填。下颌第一前磨牙根管解剖形态复杂多变,多数为单根管,但常发生形态变异,出现双根管、三根管甚至“C”型根管。这些根管变异的发生,增加了根管治疗的难度和风险。在进行根管治疗时,临床医生应熟悉其解剖变异的特点,以避免遗漏根管,导致治疗失败。首都医科大学附属北京友谊医院口腔科收治下颌第一前磨牙根管变异患牙4例,完成根
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#下颌#
38
#变异根管#
35
#变异#
36
#根管#
37
#磨牙#
38
#前磨牙#
46