Cancer Diagn Progn:化疗期间癌症相关静脉血栓栓塞的治疗策略:Keep ACT²概念
2022-04-20 “心关注”公众号 “心关注”公众号
据估计,2018年有1810万新增癌症病例和960万癌症死亡病例。虽然对可能导致癌症的因素进行预防及提高癌症筛查率,但癌症患者的数量每年仍在增加。此外,包括手术或化疗在内的癌症治疗已在全球范围内普及,
据估计,2018年有1810万新增癌症病例和960万癌症死亡病例。虽然对可能导致癌症的因素进行预防及提高癌症筛查率,但癌症患者的数量每年仍在增加。此外,包括手术或化疗在内的癌症治疗已在全球范围内普及,但完全治愈仍比较困难。
近年来,系统性化疗过程中静脉血栓的发生已成为研究热点。在接受化疗的门诊患者中,癌症相关血栓栓塞(CAT)是第二大死亡原因。由于癌症患者年龄较大,需要接受各种药物治疗,因此,药物相互作用的强度可能较高。
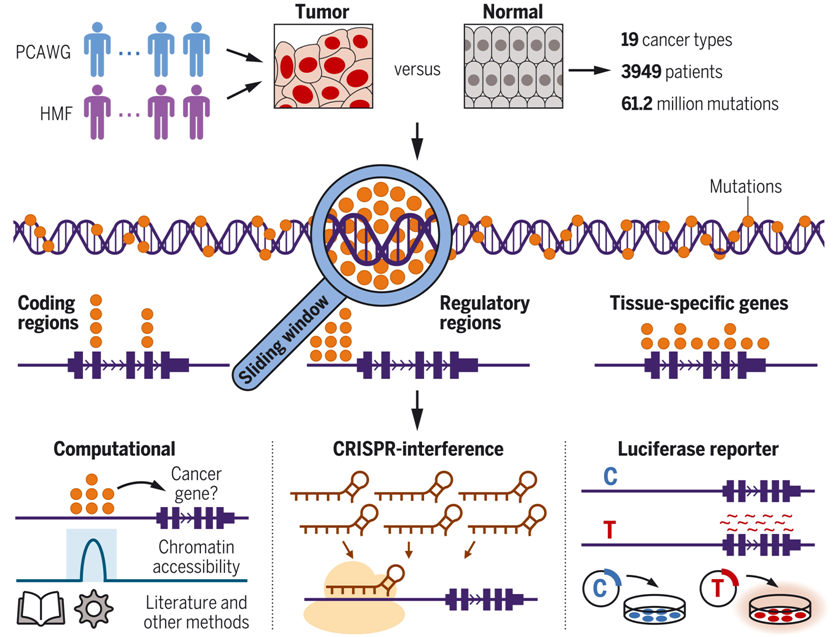
为更好的了解CAT相关机制,并采取有效治疗措施,本研究探讨了在考虑药物相互作用的情况下,继续化疗和同时进行抗凝治疗的可行性。
研究方法
研究人员回顾性评估了2017年2月至2020年12月日本岐阜县大学医学部附属医院发生胃肠道CAT的癌症患者。若患者使用艾多沙班治疗CAT并同时进行化疗后血栓消失,则被定义为Keep-ACT2(保持抗癌治疗和抗凝治疗)成功。此外,研究还评价了以细胞色素P450 (CYP)代谢为重点的艾多沙班治疗策略的有效性和安全性。
研究结果
2017年2月至2020年12月研究人员对117例接受艾多沙班治疗的胃肠癌患者CAT进行监测。除3例术后静脉血栓栓塞(VTE)外,其余114例CAT发生在化疗期间。这些患者的平均年龄为71.8±9.4岁[男性67例(58.8%),女性47例(41.2%)],平均体重为53.6±12.5 kg(表1)。在此期间,食管癌的治疗更为普遍。肺血栓栓塞(PTE)29例(25.4%),深静脉血栓形成(DVT)113例(99.1%)。1例(0.8%)患者存在PTE,但未观察到DVT。治疗前D-二聚体水平为17.1±15.9 μg/ml,治疗后为2.6±6.7 μg/ml(P<0.001)(图1)。
表1. 114例CAT患者的背景特征
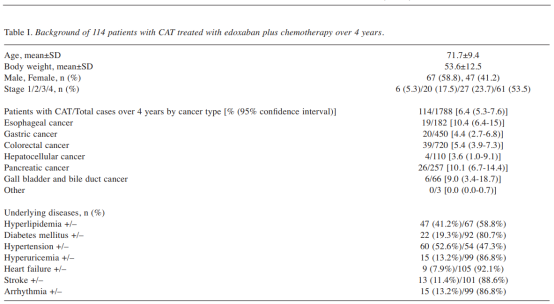

图1. D-二聚体的变化
在所有癌症患者中,Keep-ACT2成功101例(88.6%),失败13例(11.4%)(图2)。在这13例患者中,1例患者DVT的程度没有变化,6例患者DVT程度降低,D-二聚体水平正常化,但DVT仍然存在。VTE在终末期恶化,1例患者出现肿瘤出血。随癌症进展,DVT消失,但2例患者出现Trousseau综合征。2例患者D-二聚体水平和血栓体积均呈下降趋势,但均在晚期死于癌症。Keep-ACT2成功患者的不同癌症分期人数分别为I期6人,II期20人,III期27人,IV期48人;13例Keep-ACT2不成功患者的癌症分期均为IV期(P<0.001),胃癌4人,胆囊和胆管癌3人,胰腺癌4人,结直肠癌2人。
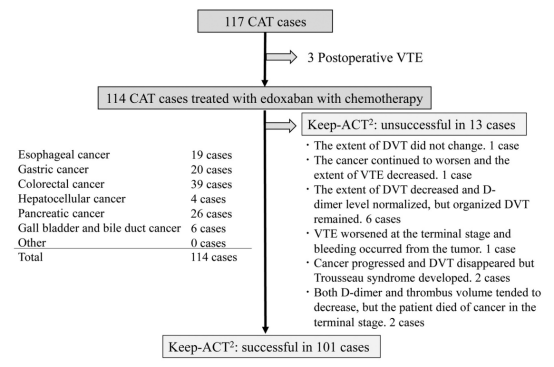
图2. Keep-ACT2在癌症患者抗凝治疗中的发生率
在化疗期间,2例使用艾多沙班的患者发生胃癌和胆管癌的局部出血;1例患者发生鼻出血并伴有化疗引起血小板减少的不良事件;1例患者在术后2月出现开胸切口处的皮下出血;以上临床相关的非大出血事件均在可接受范围内。
根据剂量减量标准,82例患者(71.9%)的使用剂量为30 mg/d,31例患者(27.2%)为60 mg/d,1例患者(0.9%)为15 mg/d。使用艾多沙班的中位月数为6个月,最长为31个月。对114名患者化疗期间受CYP代谢影响的药物数量的检查显示,所有114例患者都在使用这些药物,服用药物种类的中位数为5;正在使用受CYP代谢影响的药物多达11种(图 3)。
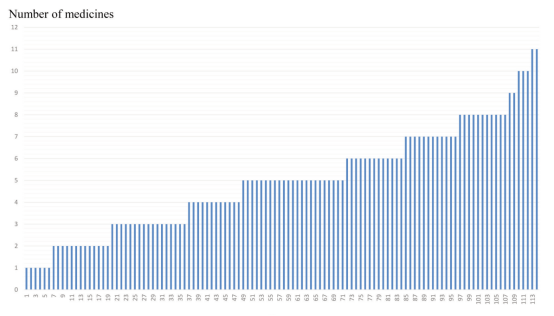
图3. 114例研究患者在化疗期间服用的由细胞色素P450代谢的药物数量
研究结论
研究中胃肠癌患者的CAT发生率并不低,化疗期间同时使用艾多沙班有助于胃肠癌患者获得持续性治疗,联合抗凝疗法具有可行性。
原始出处:
Tanaka Y, Sato Y, Suetsugu T, et al. Treatment Strategy for Cancer-associated Venous Thromboembolism During Chemotherapy: The Keep ACT2 Concept. Cancer Diagn Progn. 2021 Nov 3;1(5):417-422. doi: 10.21873/cdp.10055. PMID: 35403169; PMCID: PMC8962864.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#静脉#
38
#DIA#
45
#癌症相关#
42
#静脉血#
0
#PRO#
42