Nature Machine Intelligence:深度学习实现前列腺癌病理的高准度分析
2020-08-01 AlexYang MedSci原创
深度学习(DL)是实现组织结构数字病理识别和分类的有力方法。其在前列腺癌病理中的表现仍旧需要大量的调查。
深度学习(DL)是实现组织结构数字病理识别和分类的有力方法。其在前列腺癌病理中的表现仍旧需要大量的调查。
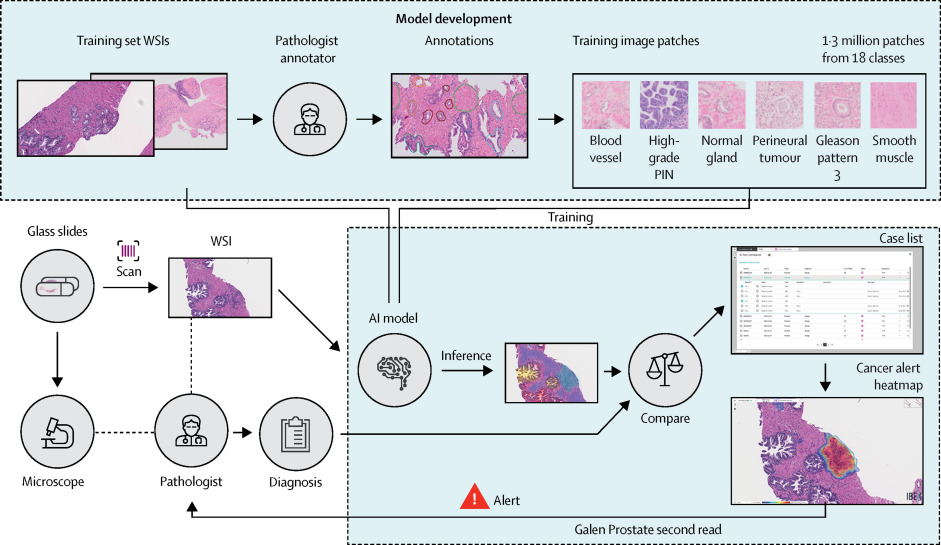
最近,有研究人员开发了基于DL的模型,用于对前列腺癌组织全切片成像进行检测。该模型基于一个大的、高质量的和已注释的训练集和一个现代最先进的卷积网络架构(NASNetLarge)。在两个验证队列中,研究人员所建立的模型的总准确度与病理学家相当,原生版本中准确度达到97.3%,使用了基于DL的增强策略时则超过98%。之后,研究人员提出了一种基于生物学意义的DL算法用于对前列腺恶性肿瘤进行格林森分级,且在一些特征良好的验证集中测试时,在患者预后分层方面具有较高的、人类水平的表现。更多的是,研究人员确定了代表整个肿瘤病灶格林森分级最优最小的肿瘤大小(大约560×560µm)。
最后,研究人员指出,他们的方法是在统一的数字病理管道中实现的,并在病理报告中能提供所有相关的肿瘤指标。
原始出处:
Yuri Tolkach, Tilmann Dohmgörgen, Marieta Toma et al. High-accuracy prostate cancer pathology using deep learning. Nature Machine Intelligence. 13 July 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#MAC#
33
#Nat#
25
#IgE#
31
前列腺癌相关研究,学习了,谢谢梅斯
40
666,学习一下,人工智能挺热的
91