Rheumatology:系统性硬化相关肺动脉高压超声诊断新思路
2021-10-06 MedSci原创 MedSci原创
系统性硬化症 (SSc) 是一种自身免疫性疾病,其特征是皮肤和内脏器官的血管损伤和纤维化。明显或亚临床的心肺受累在 SSc 中很常见。

系统性硬化症 (SSc) 是一种自身免疫性疾病,其特征是皮肤和内脏器官的血管损伤和纤维化。明显或亚临床的心肺受累在 SSc 中很常见。
大约 6% 的 SSc 患者受到肺动脉高压 (PAH) 的影响。 PAH 已成为 SSc 相关死亡的主要原因。目前可用的肺血管扩张剂疗法已显示显着提高存活率、运动能力、生活质量和肺血流动力学。尽管如此,SSc 相关多环芳烃 (SSc-PAH) 的长期预后仍然很差,中位生存期为 4 年。
本研究的目的是在一组 SSc 患者中比较超声心动图衍生的三尖瓣环平面收缩期偏移/收缩期肺动脉压(TAPSE/sPAP) 比值和 DETECT 算法之间的阳性预测值 (PPV),用于 PAH 筛查。
次要目的是确定 TAPSE/sPAP 比率与年龄、疾病持续时间、血清尿酸、FVC/DLco、NT-proBNP、DETECT 算法步骤 1 和步骤 2 之间的相关性。
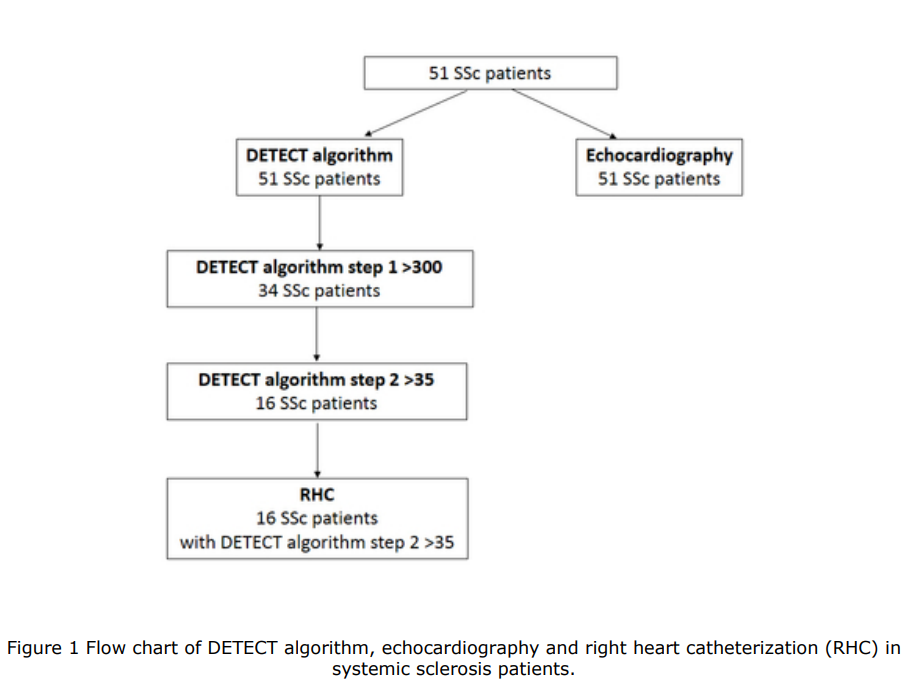
研究方法:使用 DETECT 算法和超声心动图对 51 名 SSc 患者进行 PAH 筛查。
研究结果:
超声心动图被 DETECT 算法步骤 1 推荐用于 34 名患者(66.7%)。 DETECT 算法第 2 步推荐 16 名患者(31.4%)进行右心导管插入术 (RHC)。5 名患者经 RHC 证实为 PAH。 DETECT 算法阳性预测值 (PPV) 为 31.3%。根据 DETECT 算法步骤 2,未转诊 RHC 的 SSc 患者的 TAPSE/sPAP 比值高于转诊 RHC 的 SSc 患者。使用 0.60 mm/mmHg 的临界值,8 名 (15.7%) SSc 患者的 TAPSE/sPAP 比值≤0.60 mm/mmHg。 5 名患者经 RHC 证实为 PAH。 TAPSE/sPAP 的 PPV 为 62.5%。在多元回归分析中,TAPSE/sPAP 与年龄相关。
研究结论:在 DETECT 算法第 2 步总分 >35 的 SSc 患者中,TAPSE/sPAP 比值可用于进一步选择需要 RHC 的患者以确认 PAH 诊断。
文章出处:
Colalillo A. In systemic sclerosis TAPSE/sPAP ratio can be used in addition to the DETECT algorithm for pulmonary arterial hypertension diagnosis. Rheumatology (Oxford). 2021 Oct 4:keab748. DOI: 10.1093/rheumatology/keab748. Epub ahead of print. PMID: 34605890.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#系统性#
37
#动脉高压#
39
#Rheumatology#
31
#新思路#
42
#超声诊断#
45
#超声诊断#
39
#系统性硬化#
29
学习
49
日日日撸我本身的
52